What if everything you thought about seasonal sniffles was wrong? Many people confuse two common illnesses, assuming they’re just minor inconveniences. But misidentifying them could lead to longer recovery times or even serious complications. How do you tell them apart—and why does it matter so much?
One illness often hits suddenly, leaving you drained with fever and body aches. The other creeps in slowly, starting with a scratchy throat or stuffy nose. While both are contagious, their risks differ sharply. Knowing the difference helps you act faster, protect others, and avoid unnecessary stress.
Timing plays a key role. A rapid onset usually signals a more severe condition. Gradual discomfort often points to something milder. But when should you worry? Waiting too long to address certain signs might worsen outcomes. On the flip side, overreacting to everyday congestion wastes time and resources.
This guide breaks down what to watch for, how long symptoms typically last, and steps to take if things don’t improve. You’ll learn why monitoring severity matters—and how to make informed decisions for your health.
Overview of Flu and Cold Illnesses
Have you ever wondered why some winter bugs knock you out while others just linger? Though often grouped together, these respiratory infections stem from entirely different viruses. Recognizing their distinct origins helps explain why they behave so differently in your body.
Understanding the Viral Origins and Transmission
Rhinoviruses cause most common cold cases, while influenza viruses drive the more severe illness. Both spread through tiny droplets when infected people cough, sneeze, or talk. Surfaces like doorknobs or phones can also harbor these viruses for hours.
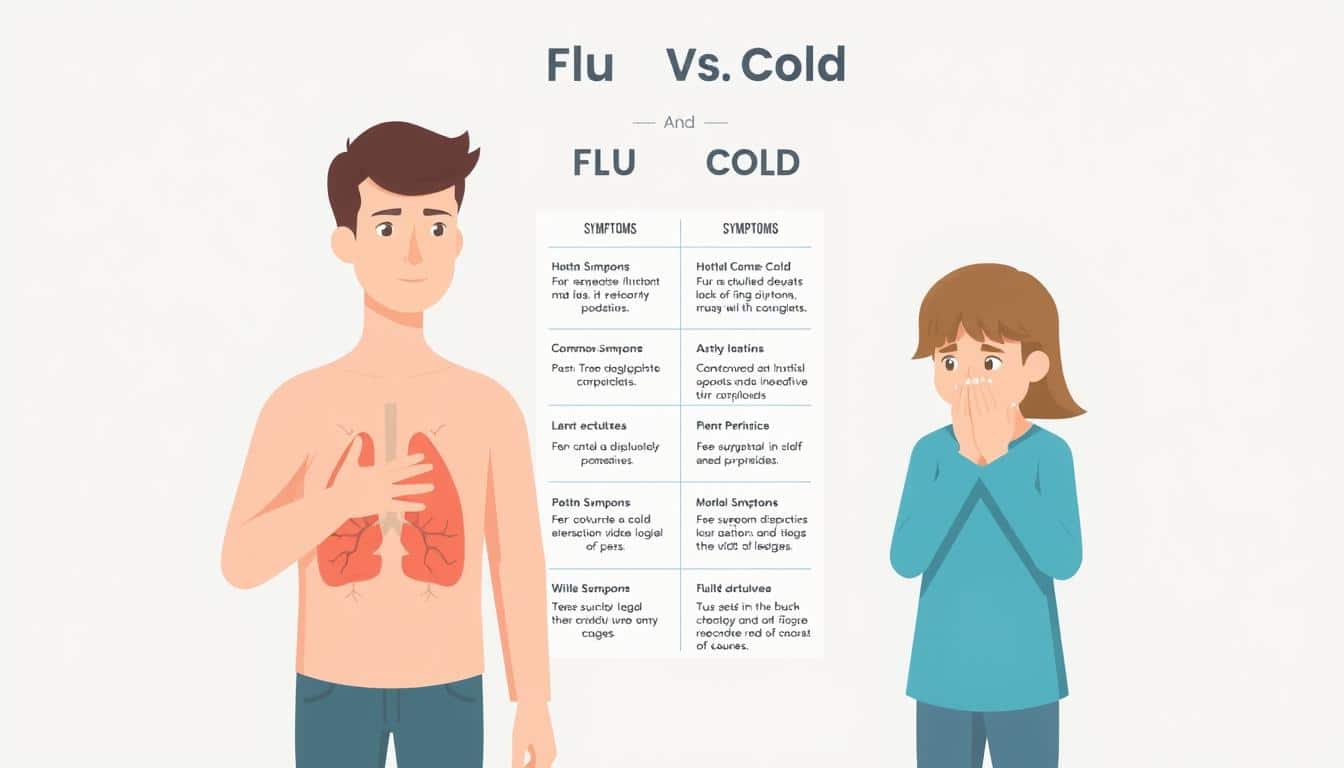
How Symptoms Typically Present in Each Illness
A sore throat and sneezing often signal the start of colds, peaking within 2-3 days. You might experience a runny nose or mild fatigue. In contrast, influenza strikes abruptly—think fever, muscle aches, and exhaustion that leaves you bedridden.
Timing matters. Cold symptoms develop gradually over 48 hours, while the other hits like a freight train. Most recover from the common cold in 7-10 days, but influenza demands longer rest. Knowing these patterns helps you respond appropriately—and protect those around you.
Flu vs Cold: Symptoms, Duration & When to Seek Help
Many confuse these respiratory illnesses early on, but quick identification matters. A sudden spike in body temperature often acts as the first red flag. If your thermometer reads above 100°F within hours, you’re likely facing a stronger virus.
Recognizing Early Signs of Each Illness
A dry, hacking cough frequently accompanies abrupt fever spikes. In contrast, mucus-filled coughs paired with a stuffy nose usually emerge gradually. Pay attention to chest discomfort—it’s more common with severe viral strains.
Body aches and chills often hit harder with certain infections. You might feel like you’ve been “hit by a truck” versus merely needing tissues. Energy levels also differ—sudden exhaustion suggests a need for immediate rest.
Timeline Variations Between Conditions
Nasal congestion from milder viruses typically eases within a week. Persistent fevers lasting 3-4 days often signal complications. Watch for color changes in mucus—yellow or green hues could indicate secondary infection.
Most people recover from standard respiratory bugs in 7-10 days. If your cough lingers beyond two weeks, consult a healthcare provider. Early action prevents minor issues from becoming major health disruptions.
Common Cold: Stages and Typical Symptoms
How does a minor throat irritation spiral into relentless congestion? Tracking the cold’s progression helps you respond strategically—and spot when ordinary recovery veers off course.
Early, Active, and Late Stage Patterns
A faint tickle in your throat marks the early phase. Within hours, sneezing starts as your body fights the virus. Mild fatigue often follows, though many push through daily tasks.
Days 3-5 bring peak misery: stuffy noses, headaches, and watery eyes. Mucus turns thicker, triggering coughs. Simple home steps—warm broths or humidifiers—ease breathing during this active stage.
By week two, symptoms wane but may leave a dry throat or lingering cough. This late phase tests patience—your body still repairs itself even after the infection fades.
When Symptoms Signal Deeper Issues
Green mucus or sinus pressure lasting 10+ days hints at bacterial complications. Unlike influenza, colds rarely cause high fevers. Watch for wheezing—it could signal bronchitis needing medical care.
Most recover with rest and hydration. Over-the-counter treatments manage discomfort, but avoid overusing decongestants. If fatigue worsens or breathing struggles emerge, consult a doctor promptly.
Understanding Flu Symptoms and Their Rapid Onset
Ever been blindsided by a health crash that feels like a switch flipped? Unlike gradual illnesses, influenza attacks your system in a dramatic way. One hour you’re functional—the next, you’re battling chills and muscle aches that demand immediate bed rest.
From Zero to Debilitated: The Flu’s Signature Speed
While colds tiptoe in, the flu slams you like a wave. Fever spikes above 101°F often hit within 4-6 hours. This abrupt way of developing symptoms leaves little time to prepare. Your joints might throb, and lifting your head could feel impossible.
Three Red Flags You Can’t Ignore
High fever acts as your body’s alarm bell. Combined with crushing fatigue and deep muscle aches, it signals a need for urgent rest. Unlike milder illnesses, these symptoms rarely ease with over-the-counter meds alone.
Pushing through flu symptoms increases your risk of pneumonia or heart strain. If fatigue lingers beyond two weeks, consult a doctor. Early intervention reduces recovery time and prevents complications that thrive on delayed care.
Risk Factors and When to Seek Medical Help
What separates a routine sniffle from a dangerous health threat? While most recover without issues, certain groups face higher risks. Quick action can prevent minor illness from escalating into emergencies.
High-Risk Groups and Critical Warning Signs
Children under five and adults over 65 often struggle to fight viruses effectively. A persistent runny nose paired with rapid breathing or bluish lips signals trouble. Chest discomfort or wheezing in these groups demands immediate attention.
Watch for dehydration signs like reduced urination or dizziness. High fevers that don’t respond to medications within 48 hours are red flags. Vulnerable individuals may develop pneumonia faster than others.
When to Contact a Healthcare Provider
Severe chest pain or pressure lasting over an hour requires urgent care. Difficulty breathing even at rest suggests possible lung complications. Confusion or sudden dizziness could indicate systemic infection.
Vaccines reduce hospitalization risks but aren’t foolproof. If symptoms worsen after initial improvement, seek help. Antiviral medications work best when started early—don’t delay testing if exposure is likely.
Trust your instincts. A lingering runny nose with fatigue might seem harmless, but combined with chest tightness, it could mask deeper issues. Early intervention saves lives—especially when viruses target weakened defenses.
Home Remedies and Treatment Tips for Flu and Cold
Minor respiratory issues can disrupt your daily rhythm, but smart self-care keeps recovery on track. Simple strategies ease discomfort while helping your body fight infections faster. Let’s explore practical ways to regain control when illness strikes.
Effective At-Home Care Practices
Rest is your top priority—it allows your immune system to work efficiently. Aim for 7-9 hours of sleep and avoid pushing through fatigue. Your health rebounds quicker when you respect your body’s limits.
Hydration thins mucus and flushes toxins. Drink water consistently, but add herbal teas or broths for variety. Warm liquids soothe sore throats while keeping dehydration at bay.
Use a humidifier to ease congestion without medications. Moist air prevents nasal passages from drying out, reducing cough frequency. This step also protects others by lowering airborne virus spread.
Medications and Recovery Boosters
Over-the-counter options like acetaminophen manage pain and fever effectively. Always follow dosage instructions—taking extra pills won’t speed up recovery. Ibuprofen reduces inflammation but consult a doctor if stomach issues arise.
Start supportive treatments at the first sign of trouble. Zinc lozenges or vitamin C supplements might shorten symptom duration when taken early. However, avoid combining multiple remedies without professional guidance.
Seek medical help if symptoms intensify after 3-4 days. Chest pain, persistent vomiting, or breathing difficulties signal it’s time for advanced care. Your health deserves proactive attention—don’t gamble with worsening conditions.
Preventive Measures: Vaccinations and Personal Care
Why gamble with your health when simple steps can shield you? Proactive strategies reduce infection risks and minimize disruptions to your daily life. Let’s explore how vaccines and smart habits create a powerful defense against seasonal threats.
Your Annual Defense Against Viral Invaders
The flu shot remains your best shield, cutting infection risk by 40-60% each year. Updated vaccines target circulating strains, making timing critical. Aim to get vaccinated by October—before the peak season hits full force.
Even if you catch the virus post-vaccine, symptoms often stay milder. This difference can mean avoiding bedrest versus struggling through weeks of fatigue. High-risk groups—like seniors or those with chronic conditions—see the most dramatic benefits.
Daily Habits That Build Resilience
Frequent handwashing breaks the chain of transmission. Use soap for 20 seconds, especially after touching shared surfaces. Carry alcohol-based sanitizer for times when sinks aren’t available.
Boost your body’s natural defenses with plenty of sleep and nutrient-rich foods. Hydration keeps mucous membranes robust against invaders. Regular exercise maintains muscle strength, which supports immunity and faster recovery.
Disinfect phones, keyboards, and doorknobs during cold/flu season. Avoid touching your face—this simple habit slashes infection odds by 34%. Pair these steps with vaccines, and you’ll navigate each year’s risks with confidence.
Conclusion
Could your health decisions today prevent weeks of downtime tomorrow? Recognizing whether you’re facing a sudden viral assault or gradual congestion changes everything. The key lies in timing—one strikes like lightning, while the other creeps in like fog.
Prioritize your body’s signals. Rest becomes non-negotiable during the first critical week, whether battling intense fatigue or mild sniffles. Hydration with water, broths, or electrolyte-rich fluids supports your system’s fight against invaders.
Track progress daily. Lingering issues beyond seven days—especially chest tightness or recurring fever—demand professional input. Your body often heals itself with proper care, but stubborn symptoms need smarter strategies.
Stay vigilant, not anxious. Simple choices—extra sleep, steady fluids, symptom logging—empower recovery. When in doubt, trust that seeking clarity beats guessing. Your health deserves this balanced approach every week of the year.