You’ve been feeling tired. Not just “end-of-a-long-week” tired, but a deep, persistent exhaustion that coffee just doesn’t touch. Or maybe you’ve noticed you’re bruising more easily than usual. These are common reasons people come to see me, and often, a simple blood test can give us some clues. When we look at those results, we’re often looking at the products of a remarkable, ongoing process in your body called hematopoiesis. It’s a big word, I know, but it simply means blood cell production. Your body is constantly making new blood cells, day in and day out, and it’s a process that’s absolutely essential for life.
So, What Exactly is Hematopoiesis?
Alright, let’s break down that term: hematopoiesis (heh-ma-tuh-poy-EE-sus). It sounds a bit like a spell from a fantasy novel, doesn’t it? But it’s very real and happening inside you right now. “Haima” comes from Greek for blood, and “poiesis” means “to make something.” So, hematopoiesis is literally “to make blood.” It’s the continuous, vital cycle where your body manufactures all the different types of blood cells you need to stay healthy. This isn’t a one-time event; it starts even before you’re born and keeps going your whole life. You might also hear it called hemopoiesis, but it’s all the same amazing process.
The Stars of the Show: What Blood Cells Are We Talking About?
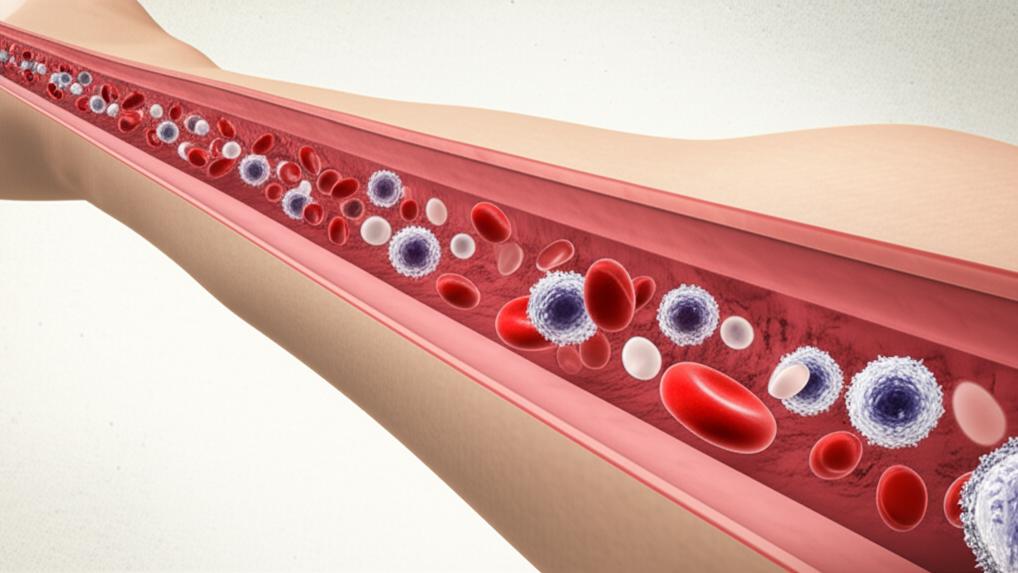
When we talk about hematopoiesis, we’re talking about the creation of all the crucial components of your blood. Each has a special job.
Red Blood Cells (Erythrocytes): Your Oxygen Couriers
First up are your red blood cells, or erythrocytes. Think of these as tiny delivery trucks. Their main job? To pick up oxygen from your lungs and deliver it to every organ and tissue in your body. They also cart away carbon dioxide, bringing it back to your lungs so you can breathe it out. You have more of these than any other blood cell. The specific process of making red blood cells is called erythropoiesis.
White Blood Cells (Leukocytes): Your Body’s Defense Team
Next, we have white blood cells, or leukocytes. These are your internal bodyguards. They’re on constant patrol, fighting off infections from germs like bacteria and viruses, and they also help destroy any abnormal cells. Making these defenders is called leukopoiesis.
There are a few main types, each with a slightly different role:
- Neutrophils, Basophils, and Eosinophils: These are often grouped as granulocytes and are usually first responders to infection or inflammation.
- Monocytes: These are like the cleanup crew, tidying up damaged cells and also fighting invaders.
- Lymphocytes: These are more specialized fighters. You’ve got B-cells (which make antibodies), T-cells (which directly attack infected cells or regulate the immune response), and natural killer cells.
Platelets (Thrombocytes): The Clotting Crew
Finally, there are platelets, or thrombocytes. These aren’t fully-fledged cells but rather tiny fragments of cells. If you get a cut or injury, these little guys rush to the scene. They’re sticky, and they clump together to form a clot, sealing up the damage and stopping you from losing too much blood. The making of platelets is called thrombopoiesis.
Where Does All This Blood-Making Magic Happen?
The main headquarters for hematopoiesis is deep inside your bones, in a spongy tissue called bone marrow. When blood cell production happens here, it’s called medullary hematopoiesis. Once the new cells are ready, they’re released from the bone marrow into your bloodstream to get to work.
Sometimes, if the bone marrow isn’t up to the job, other organs like your liver and spleen can step in. This is called extramedullary hematopoiesis. It’s more common in certain situations or if there’s a problem.
The location actually changes as we develop:
Before We’re Born
It’s pretty amazing – blood cell production starts super early, when an embryo is still developing.
- Around week 3 of pregnancy, the yolk sac (a structure that nourishes the early embryo) starts making some early forms of red blood cells.
- By months 2 and 3, the liver and spleen take over much of the red blood cell and platelet production. The liver, spleen, and another little organ called the thymus start making white blood cells.
- By about month 5 of pregnancy, the bone marrow becomes the primary site, though the thymus and spleen still help out with some white blood cells.
After Birth and Throughout Life
From the moment we’re born and all through adulthood, most of our blood cells are made in our bone marrow. Certain lymphocytes, those specialized white blood cells I mentioned, also mature in the thymus gland (it’s just behind your breastbone).
If something goes wrong with the bone marrow – say, due to a disease – the body can sometimes try to shift production back to those earlier sites like the liver, spleen, or lymph nodes. It’s like having backup factories.
The Journey of a Blood Cell: How Hematopoiesis Works
So, how does one “master cell” become all these different types of blood cells? It’s a fascinating journey.
From Stem Cell to Specialized Cell
It all begins with a very special kind of cell called a hematopoietic stem cell (HSC). Think of this as the ultimate ancestor cell, the one that can become any type of blood cell. These HSCs are incredible because they can both make copies of themselves (so you don’t run out) and also start down a path to become a more specialized cell.
An HSC first develops into what we call a precursor cell, or sometimes a “blast” cell. This cell is committed to becoming a certain type of blood cell, but it’s still young and immature. It then goes through several stages of dividing and changing, getting more and more specialized until it’s a fully mature, ready-to-work red blood cell, white blood cell, or platelet.
Making Red Blood Cells (Erythropoiesis)
For red blood cells, an HSC in your bone marrow matures into a precursor called an erythroblast. This then becomes an immature red blood cell known as a reticulocyte. You might see reticulocyte counts on a blood test; they tell us how actively your bone marrow is making new red cells. Finally, the reticulocyte matures into a full-fledged red blood cell.
Crafting White Blood Cells (Leukopoiesis)
White blood cells are a bit more varied.
- Granulocytes (Neutrophils, Eosinophils, Basophils): These guys develop from HSCs along what’s called the myeloid cell line (myeloid just means related to the bone marrow). The HSC becomes a myeloblast, then a myelocyte, and then differentiates into one of the three types of granulocytes.
- Monocytes: These also come from the myeloid line in the bone marrow. The HSC becomes a monoblast before maturing into a monocyte.
- Lymphocytes (B-cells, T-cells, Natural Killer cells): These develop along a different path, the lymphoid cell line, as they originate in lymph tissue (which includes bone marrow, but also the thymus and other areas). HSCs become lymphoblasts, which then specialize into T-cells, B-cells, or natural killer cells. Some of these, like T-cells, actually travel from the bone marrow to the thymus to finish their training. Pretty cool, right?
Producing Platelets (Thrombopoiesis)
Platelets also start with an HSC in the bone marrow. This matures into a megakaryoblast, which then grows into a very large cell called a megakaryocyte. Instead of dividing into new cells, this giant megakaryocyte actually shatters into tiny pieces, and those fragments are your platelets.
How Long Does This Process Take?
Your body is pretty smart; it adjusts blood cell production based on your needs. For instance, if you pick up an infection, your body will ramp up white blood cell production to fight it off. Generally, hematopoiesis is a continuous cycle timed to replace cells as they wear out.
On average:
- Red blood cells live for about 120 days.
- White blood cells have a shorter lifespan, from just a few hours to a few days, depending on the type and if they’re actively fighting something.
- Platelets stick around for about five to nine days.
When Hematopoiesis Goes Off Course
Now, this beautifully regulated system of hematopoiesis can sometimes run into trouble. When that happens, you can end up with too few or too many of certain blood cells, leading to various health issues. It’s all about balance.
Too Few or Too Many Red Blood Cells
- Anemia: This is when you have too few red blood cells. Since they carry oxygen, a shortage means your body’s tissues aren’t getting enough. This often leads to that persistent tiredness, weakness, or even shortness of breath I mentioned earlier.
- Erythrocytosis: This is the opposite – too many red blood cells. While it might sound good to have extra, it can make your blood too thick, increasing the risk of clots, heart attack, or stroke. Mild cases might just cause some discomfort.
White Blood Cell Imbalances
- Leukopenia: This means too few white blood cells. Because these are your infection fighters, a low count can make you more vulnerable to getting sick.
- Leukocytosis: This is when you have too many white blood cells. Often, this is a sign your body is fighting an infection, which is normal. But sometimes, a persistently high count can point to a blood disorder or even certain cancers.
Platelet Problems
- Thrombocytopenia: Too few platelets. This can mean your blood doesn’t clot properly, so you might bruise very easily or experience prolonged bleeding from minor cuts.
- Thrombocytosis: Too many platelets. This can increase your risk of forming unnecessary and potentially dangerous blood clots.
What Can Disrupt Hematopoiesis?
Several things can throw a wrench in the works of hematopoiesis.
- Aging: As we get older, sometimes more fat can deposit in our bone marrow, leaving less room for blood cell production. It’s a natural part of aging for some.
- Blood disorders and Cancers: Conditions like leukemia, lymphoma, and myeloma directly affect blood cell production, often leading to an overproduction of abnormal, non-functional cells or a shortage of healthy ones.
- Medications: Some treatments, while necessary, can impact hematopoiesis. A common example I see in my practice is chemotherapy. It’s designed to kill fast-growing cancer cells, but it can also affect the fast-growing cells in your bone marrow, sometimes leading to low white blood cell counts (a condition called neutropenia).
When we suspect a problem with hematopoiesis, we’ll often start with blood tests. Depending on what we find, we might need to do further investigations, like a bone marrow biopsy, where a small sample of bone marrow is taken (usually from the hip bone) and looked at under a microscope by a specialist called a pathologist. They can see the cells in their “factory” and get a clearer picture of what’s going on. We’ll discuss all options and what they mean for you.
Take-Home Message: Understanding Your Blood
It’s a lot to take in, I know! But understanding a bit about hematopoiesis can help you make sense of your health and any tests we might run. Here are the key things to remember:
- Hematopoiesis is your body’s continuous process of making all types of blood cells.
- It mainly happens in your bone marrow, starting from hematopoietic stem cells.
- The three main types of blood cells produced are red blood cells (for oxygen), white blood cells (for immunity), and platelets (for clotting).
- Problems with hematopoiesis can lead to having too few or too many of these cells, causing conditions like anemia, increased infection risk, or clotting issues.
- Various factors, from aging to diseases like leukemia or certain medications, can affect this vital process of hematopoiesis.
This whole system is incredibly complex and usually works without us even thinking about it. It’s one of the many marvels of the human body.
You’re not alone in navigating these concerns. If you ever have questions about your blood health or test results, please don’t hesitate to ask. That’s what we’re here for.