Have you ever brushed off pelvic discomfort as “just a bad period” or stress? Many women do—but what if that lingering ache holds clues to your health? Lower abdominal pain isn’t always routine. It can range from mild twinges to sharp, persistent warnings demanding attention.
Understanding the nature of these sensations helps you act wisely. Symptoms may appear suddenly (acute) or linger for months (chronic). Sharp cramps could point to ovarian issues, while dull pressure might relate to digestive or urinary systems. Don’t dismiss discomfort—even sporadic pains may reveal conditions like endometriosis or cysts.
Accurate symptom tracking matters. Note when pain occurs: during ovulation? After meals? Does movement ease it? These details help doctors narrow causes faster. While some cases resolve with rest, others require urgent care—like appendicitis or ectopic pregnancy.
This section guides you through decoding your body’s signals. You’ll learn why timing, location, and intensity matter—and when to consult a healthcare provider. Knowledge transforms vague worries into actionable steps for better pelvic health.
Understanding Lower Abdominal Pain: An Overview
How often do you dismiss pelvic discomfort as temporary? The sensations in your abdomen vary widely—from subtle pressure to waves of intense cramping. Recognizing these differences helps you identify potential health concerns early.
What Lower Abdominal Pain Feels Like
Discomfort might manifest as throbbing, stabbing, or a persistent ache. Sharp bursts often signal acute issues like infection or organ inflammation, while dull pressure could relate to chronic disease. Some describe it as a twisting sensation near the bladder or ovaries.
Recognizing Common Symptoms
Watch for patterns beyond physical pain. Bloating paired with nausea often points to digestive issues. Fever or chills may indicate infections affecting urinary or reproductive organs. Sudden cramping during movement could reveal cysts or muscle strain.
Tracking symptom duration matters. A three-day ache differs from recurring monthly episodes. Always note accompanying signs—like changes in bowel habits or urinary urgency. These details help doctors pinpoint causes faster, whether linked to your intestines, uterus, or kidneys.
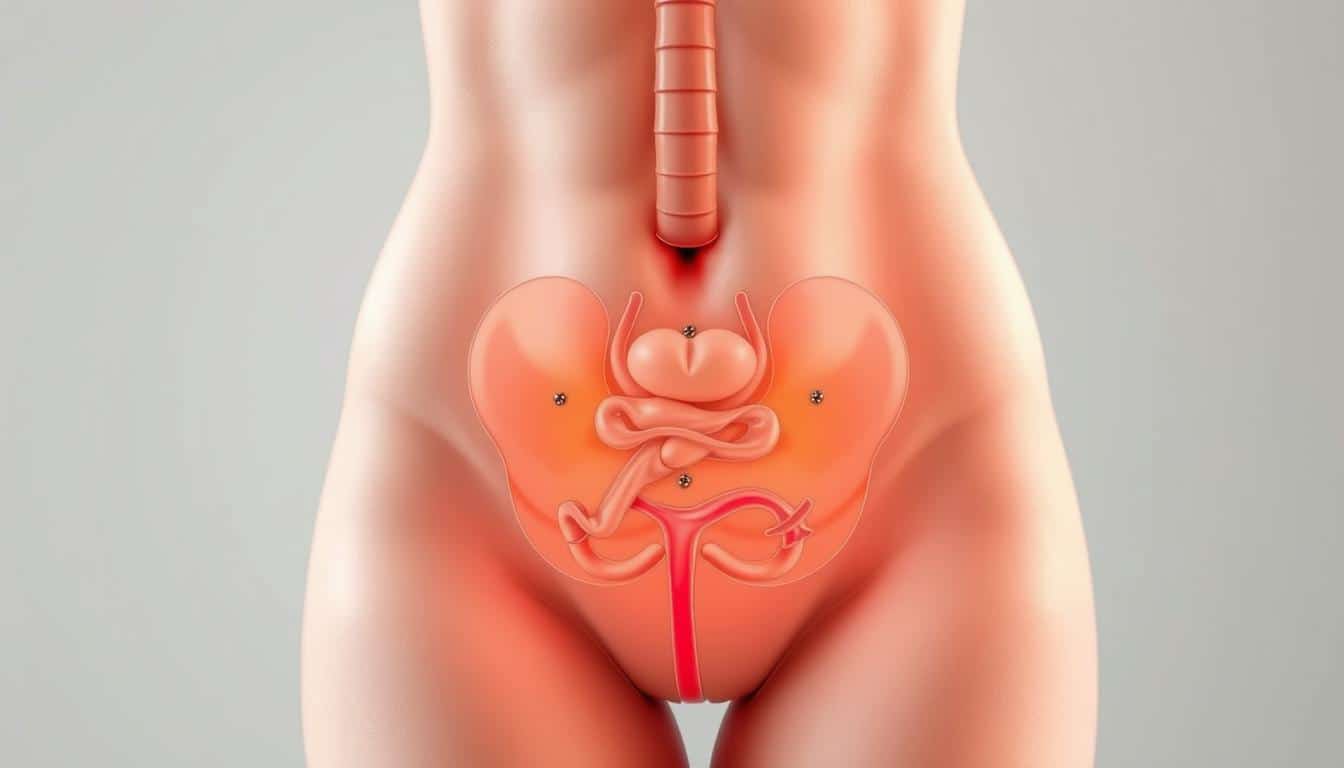
Potential Causes in the Female Reproductive System
Could your recurring cramps be signaling more than just your period? Many pelvic discomfort patterns trace back to the uterus and surrounding reproductive organs. These issues often involve hormonal shifts, tissue growth, or structural changes that impact your overall health.
Menstrual Cramps and Dysmenorrhea
Monthly cramping occurs when the uterus contracts to shed its lining. For some, this feels like a dull ache. Others experience sharp, wave-like spasms lasting days. Severe cases (dysmenorrhea) may stem from high prostaglandin levels or underlying conditions.
Track symptom timing. Pain starting 1-2 days before bleeding often aligns with typical cycles. Discomfort persisting beyond your period warrants attention. Your body might hint at inflammation or hormonal imbalances needing care.
Endometriosis, Adenomyosis, and Fibroids
Endometriosis develops when uterine-like tissue grows outside the uterus, causing inflammation. Adenomyosis involves this tissue penetrating the uterine wall. Both conditions create pelvic pressure and stabbing pains during cycles.
Fibroids—noncancerous growths in the uterus—often cause heaviness or bloating. Large ones may press on nearby organs. These three types of reproductive issues frequently coexist, complicating diagnosis without imaging tests.
Persistent symptoms like bleeding between periods or pain during intimacy should prompt a health evaluation. Early intervention helps manage these conditions before they affect fertility or daily life.
Digestive and Urinary Contributors to Abdominal Pain
Your body’s plumbing systems—digestive and urinary—often play starring roles in pelvic discomfort. While reproductive health grabs attention, these interconnected networks can trigger persistent symptoms that radiate across your lower abdomen.
Gastrointestinal Issues: IBS, Constipation, and Diverticulitis
Chronic constipation creates pressure as waste builds up, stretching intestinal walls. This causes lower abdominal cramping that worsens with inactivity. Conditions like IBS amplify sensitivity—gas or mild bloating may feel like stabbing pains.
Diverticulitis inflames small intestinal pouches. Sharp discomfort typically concentrates on the left side but can spread. Fever or nausea often accompanies flare-ups, signaling infection needing prompt care.
Urinary Tract Infections and Kidney Stones
Urinary tract infections irritate bladder lining, producing burning sensations and urgent bathroom trips. Left untreated, bacteria may ascend to kidneys, escalating pain to your back or sides.
Kidney stones trigger sudden, severe spasms as crystals move. You might notice blood-tinged urine or difficulty sitting still. While small stones pass naturally, larger ones require medical intervention to prevent complications.
Both systems share nerve pathways with reproductive organs, sometimes masking the true cause. Track patterns: Does pain spike after meals or hydration? Are bowel movements irregular? These clues help distinguish between gut-related distress and pelvic inflammatory conditions.
Evaluating Pain: Central, Left-Sided, and Right-Sided Differences
Where you feel discomfort can reveal critical clues about its origin. Central aches near the belly button often stem from early-stage appendicitis or intestinal inflammation. As conditions progress, pain may shift—like appendicitis migrating to the lower right quadrant.
Lower Left Abdominal Pain Considerations
Left-sided discomfort frequently links to the bowel. Diverticulitis flares here, causing sharp pains worsened by movement. Gas buildup or constipation may mimic these sensations but usually resolves faster.
On the opposite side, persistent lower right pain demands attention. Appendicitis often starts as a dull ache near the belly button before concentrating in this area. Ovarian cysts or ectopic pregnancy can also trigger one-sided cramping.
Reproductive issues sometimes overlap with digestive symptoms. For example, a twisted ovary might feel like sudden intestinal spasms. Track whether discomfort correlates with meals, cycles, or bladder activity. This helps your care team separate system-specific causes.
Always note patterns: Does leaning forward ease pressure? Is there blood in stool or urine? These details matter more than intensity alone. While some side-specific pains resolve with rest, others—like appendicitis—require swift intervention to prevent complications.
How to Recognize and Manage Severe Abdominal Pain
When does discomfort cross from manageable to urgent? Severe pelvic distress often announces itself through unmistakable signals your body can’t ignore. Recognizing these red flags helps you act swiftly to protect your health.
Warning Signs That Require Immediate Care
Persistent vomiting paired with cramping often indicates blocked intestines or infections. If you can’t keep fluids down for over 12 hours, dehydration risks spike. Blood in stool or urine—whether bright red or dark—signals potential bleeding in your digestive tract or bladder.
Sudden, knife-like pains that worsen when moving demand attention. These could reveal ruptured cysts, kidney stones, or appendicitis. Fever above 101°F with pelvic pressure may point to severe infections like pyelonephritis.
Don’t overlook urinary symptoms. Burning during urination with flank pain suggests advancing tract infections. Inability to empty your bladder fully creates dangerous pressure buildup requiring catheterization.
Time-sensitive conditions like ectopic pregnancy or ovarian torsion need rapid treatment to prevent organ damage. Track symptom progression: Does pain intensify despite rest? Are over-the-counter meds ineffective? These patterns help ER teams prioritize scans or surgery.
Delaying care for severe cases risks sepsis, internal scarring, or fertility issues. Trust your instincts—if symptoms feel alarming, seek evaluation. Early intervention transforms outcomes for many abdominal conditions.
Home Remedies and Self-Care Strategies for Relief
What if simple home adjustments could ease your discomfort? While some causes require medical care, many mild symptoms respond well to targeted self-care. Start by identifying patterns—does your belly ache spike after certain foods or activities?
Effective At-Home Pain Relief Options
Heat therapy works wonders for cramping. Try a warm compress on your lower torso for 15-minute intervals. Over-the-counter anti-inflammatories like ibuprofen reduce swelling linked to menstrual cycles or muscle strain.
Stay hydrated—dehydration worsens constipation and bladder irritation. Herbal teas with ginger or peppermint soothe digestive upset. For gas-related pressure, gentle clockwise belly massage often brings relief.
Lifestyle Adjustments and Preventive Measures
Adjust your diet if you notice recurring issues. High-fiber foods prevent constipation, while probiotic yogurt fights harmful bacteria. Limit caffeine and alcohol during your period to reduce inflammation.
Stress management matters. Daily walks and deep breathing exercises lower cortisol levels that aggravate gut sensitivity. Track symptoms in a journal—note foods, activities, and pain intensity.
When to seek help: If fever accompanies sharp right-sided belly pain—a possible appendicitis sign—discontinue home care immediately. Sudden weight loss or blood in stool also warrants professional evaluation. Most people find these strategies manage occasional flare-ups effectively while preventing new episodes.
Lower Abdominal Pain in Women: What It Could Mean – A Diagnostic Perspective
Recognizing when pelvic discomfort signals deeper issues requires understanding diagnostic red flags. Doctors often start by evaluating symptom patterns that differentiate routine aches from urgent conditions.
Identifying Key Warning Signs
Kidney-related issues often surface through flank pain, fever, or blood in urine. Sudden weight loss paired with persistent fatigue could indicate systemic problems needing scans or blood tests.
A tender area near your belly button that worsens when pressed might suggest appendix inflammation. This “McBurney’s point” tenderness often precedes nausea and requires immediate imaging to confirm appendicitis.
Distinct types of urinary tract infections behave differently. Lower UTIs cause burning, while upper infections affect kidneys and trigger back pain. Recurrent episodes may warrant urine cultures to identify resistant bacteria.
Unexplained appetite loss or drastic weight changes often accompany serious gastrointestinal or reproductive conditions. Diagnostic steps might include ultrasounds to check for ovarian cysts or CT scans for intestinal blockages.
Never ignore sudden pain shifts. If discomfort migrates from the belly button to the lower right side, your appendix might be at risk. Early diagnosis of these patterns prevents complications like rupture or sepsis.
Conclusion
Pelvic discomfort often speaks volumes when you know how to listen. From reproductive concerns like ectopic pregnancy to urinary tract infections, your body’s signals guide next steps. Digestive imbalances and muscular strain also contribute, requiring careful symptom tracking.
Early evaluation matters. Sharp cramping paired with fever could indicate a urinary tract infection, while one-sided pelvic pressure might signal ectopic pregnancy. Note patterns: Does rest ease discomfort? Are there sudden changes in bathroom habits?
Use this knowledge proactively. Mild cases may improve with hydration or heat therapy, but persistent issues need professional insight. Conditions like ectopic pregnancy demand swift imaging tests to prevent complications. Similarly, recurring urinary tract infections often require targeted antibiotics.
Your health thrives on partnership. Track symptoms, ask questions, and share observations with your care team. Whether managing chronic discomfort or sudden flares, informed decisions protect your well-being. Stay curious, stay empowered—your body’s whispers often hold the answers.