Imagine this: you’re enjoying a spring picnic, sun shining, birds singing. Suddenly, your nose starts to run, your eyes itch like crazy, and a patch of hives pops up on your arm. What’s going on? Or perhaps you’ve heard of someone who has a severe reaction to a bee sting, their throat tightening, feeling faint. These dramatic, and sometimes scary, bodily responses often have tiny, powerful cells at their heart: mast cells. They’re usually unsung heroes, but when they get a bit… enthusiastic, we certainly know about it.
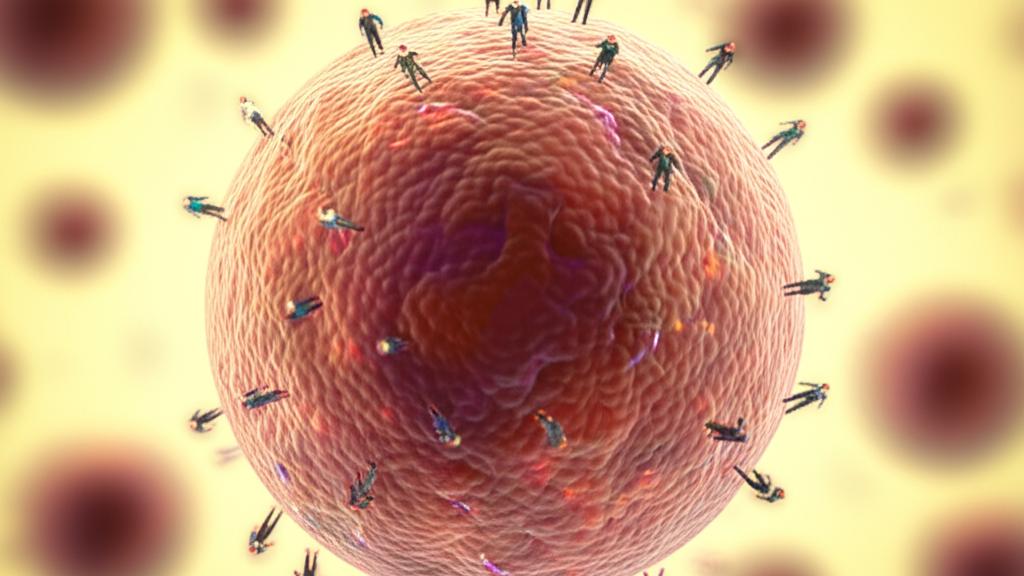
So, what exactly are these mast cells? Think of them as your body’s highly alert security guards. They’re a special type of white blood cell, born in your bone marrow – that spongy stuff inside your bones. From there, they travel through your bloodstream and set up shop in your body’s tissues, especially places that are first-line defenders against the outside world. We’re talking about your skin, your airways, your gut. They’re there to protect you from genuine threats like pathogens (nasty invaders like viruses or bacteria) and toxins, like the venom from a bee sting.
These little guards don’t usually go looking for trouble directly. Instead, they sit tight in the tissues, waiting for a signal.
It’s a fascinating system. When other immune cells, like B cells, spot an invader (or something they think is an invader, like pollen), they create special “wanted posters” called antibodies, specifically a type known as Immunoglobulin E (IgE). These IgE antibodies then latch onto the surface of your mast cells. It’s like they’re priming the alarm.
The next time that same substance – say, that pollen or bee venom – enters your body, the IgE already on your mast cells grabs onto it. Wham! The alarm goes off. This is called mast cell activation.
When activated, mast cells release a whole cocktail of potent chemicals they’ve been storing in tiny sacs called granules. This process is called degranulation. The most famous chemical in this mix is histamine.
Histamine is powerful stuff. It causes a cascade of events:
- Your blood vessels widen and become a bit leaky. This helps other immune cells rush to the scene.
- Fluid can build up in the area, leading to swelling.
- You might start producing more mucus.
- The smooth muscles in your airways and your gut can contract, trying to push out whatever’s causing the problem.
This is why you might get:
- Flushed, itchy skin or hives.
- A runny nose, sneezing, or a cough.
- Sometimes, an upset stomach, diarrhea, or even vomiting.
In really severe cases, this activation can lead to anaphylaxis – a life-threatening reaction where your airways can swell shut and your blood pressure can plummet. Scary, I know, but important to understand.
But it’s not all drama! Mast cells also have a day job in keeping things running smoothly, what we call homeostasis. They play a part in things like:
- The growth of new blood vessels.
- Bone growth and repair.
- Helping cells in your airways grow and heal.
You won’t find many mast cells just cruising around in your blood. They prefer to be stationed where the action is likely to happen. That’s why they’re concentrated in:
- Your skin.
- The tissues lining your airways and lungs.
- Your gastrointestinal (GI) tract – your stomach and intestines.
They also hang out around blood vessels and nerves.
If you could peek inside a mast cell, you’d see a central control room (the nucleus) surrounded by hundreds of these little storage granules. These granules are packed with those chemical messengers, or mediators:
- Histamine: We’ve talked about this one – the itch-maker, the vessel-opener.
- Proteases: These are enzymes like tryptase and chymase. They help break down tissue a bit so other immune cells can get where they need to go. You might hear about tryptase levels in certain blood tests.
- Cytokines and chemokines: These are like little text messages that call in reinforcements, tell other immune cells to multiply, and help guide them to the trouble spot.
- Heparin: This substance helps prevent blood clots, which can also help keep pathways open for immune cells.
Mast cells also have many different “docking stations” or receptors on their surface. The IgE receptor is the most famous one for allergies, but they have others that can recognize different signals, some even spotting pathogens directly or responding to other types of antibodies.
What Happens When Mast Cells Go Rogue? Common Mast Cell Issues
Sometimes, these usually helpful mast cells can become a bit overzealous or their numbers can get out of whack. This can lead to a few different issues.
Some common problems where mast cells play a starring (and often unwelcome) role include:
- Environmental allergies: Think hay fever, pet allergies.
- Asthma: Especially allergic asthma.
- Food allergies.
- Hives (urticaria): Those itchy welts.
Then there are some rarer conditions:
- Mast Cell Activation Syndrome (MCAS): This is a tricky one. In MCAS, people experience repeated episodes of allergy-like symptoms, sometimes even anaphylaxis, but often without a clear, identifiable trigger. It can be quite a diagnostic journey.
- Mastocytosis: This is a condition where the body makes too many mast cells, and they can build up in the skin, bone marrow, or other organs.
- Hereditary alpha-tryptasemia: This is a genetic condition some people are born with, causing them to have higher baseline levels of tryptase (that enzyme from mast cells) in their blood. Interestingly, many people with this don’t have any symptoms at all, but for some, it might make allergic-type reactions more likely or more intense.
What might you notice? Symptoms of Mast Cell Overactivity
When mast cells are overactive, that release of histamine and other mediators can cause a whole range of symptoms. You might experience:
- Skin changes: Flushing (skin suddenly getting red and hot), intense itching, or hives.
- Swelling (edema): This can happen in various parts of the body.
- Breathing troubles: Feeling short of breath, wheezing.
- Abdominal issues: Cramps, nausea, vomiting, diarrhea.
- Brain fog or fatigue.
- Episodes that feel like severe allergic reactions, sometimes leading to anaphylaxis.
Figuring It Out: Tests and Diagnosis
If you’re having symptoms that make us think about mast cell issues, we’ll want to investigate. It’s a bit like detective work. We might suggest:
- Blood tests: We can look for markers of mast cell activation, like tryptase. Sometimes we measure this during a symptomatic episode and then again when you’re feeling well, to compare. We can also do blood tests for specific allergies (those IgE antibodies).
- Urine tests: Certain breakdown products of mast cell mediators can be found in your pee.
- Allergy skin testing: To help identify specific triggers if an allergy is suspected.
- Biopsies: In some cases, especially if mastocytosis is suspected, a small sample of tissue (like skin or from the GI tract during an endoscopy, or even bone marrow) might be taken. A pathologist – a doctor who specializes in looking at cells and tissues under a microscope – will then examine it for an increased number of mast cells or abnormal-looking ones.
- Genetic testing: This might be considered if something like hereditary alpha-tryptasemia is on the radar.
It can take time to piece the puzzle together, especially with conditions like MCAS.
Managing Mast Cell Mayhem: Treatments
If we find that your mast cells are indeed causing trouble, the goal is to calm things down and manage your symptoms. Treatment really depends on what’s going on. Options can include:
- Avoiding known triggers: If specific allergens are identified, doing your best to avoid them is key. Easier said than done sometimes, I know!
- Medications to manage symptoms:
- Medications for severe reactions/anaphylaxis:
- For mastocytosis: If it’s a more aggressive form, treatments might involve cytoreductive therapy (medications to reduce cell numbers, sometimes similar to chemotherapy).
We’ll always sit down and talk through the best plan for you and your specific situation. It’s about finding what gives you the best quality of life.
So, Are Mast Cells Good or Bad?
It’s easy to hear all this and think mast cells are just troublemakers, right? Especially if you’re the one dealing with the itchy hives or the scary allergic reaction. But truly, most of the time, they are absolutely essential. They’re on our side, defending us from real dangers and helping keep our bodies in balance. It’s just that sometimes, like an overenthusiastic security guard, they can misinterpret a situation or react a bit too strongly.
Take-Home Message: Key Things to Remember About Mast Cells
Alright, let’s boil it down. If there are a few key things to remember about mast cells, it’s these:
- Mast cells are key immune cells, your body’s first responders, primarily living in tissues like your skin, airways, and gut.
- They activate in response to threats (like infections or toxins) or perceived threats (allergens), releasing chemicals like histamine.
- This release causes allergy symptoms and, in severe cases, anaphylaxis.
- When mast cells are overactive or too numerous, it can lead to conditions like allergies, asthma, MCAS, or mastocytosis.
- Diagnosis involves looking for signs of mast cell activation and identifying triggers.
- Treatments aim to avoid triggers, manage symptoms with medications like antihistamines and mast cell stabilizers, and have emergency plans for severe reactions involving mast cells.
A Final Thought
If you’re struggling with symptoms that make you wonder about your mast cells, please know you’re not imagining things, and you’re certainly not alone. It can be a complex area of medicine, but we’re here to help you figure it out and find ways to feel better. Don’t hesitate to bring up your concerns.