What if your most fertile days aren’t when you think? Understanding your body’s rhythms could be the key to unlocking your conception journey. This guide offers science-backed clarity for anyone navigating the complexities of reproductive health.
Your monthly cycle holds patterns that reveal critical insights. From menstruation to mid-phase hormonal shifts, each stage plays a role in fertility. Medically reviewed strategies from experts like Dr. Charlsie Celestine help demystify these biological processes.
You’ll discover how to identify subtle physical cues that signal prime conception windows. We break down tracking methods that go beyond basic calendar calculations, including temperature monitoring and hormonal changes. These tools empower you to make informed decisions.
Backed by Flo Health’s research, this resource prioritizes accuracy without overwhelming jargon. Whether you’re new to cycle awareness or refining existing knowledge, the guidance here adapts to your needs. Ready to transform uncertainty into actionable clarity?
Understanding Your Menstrual Cycle and Ovulation
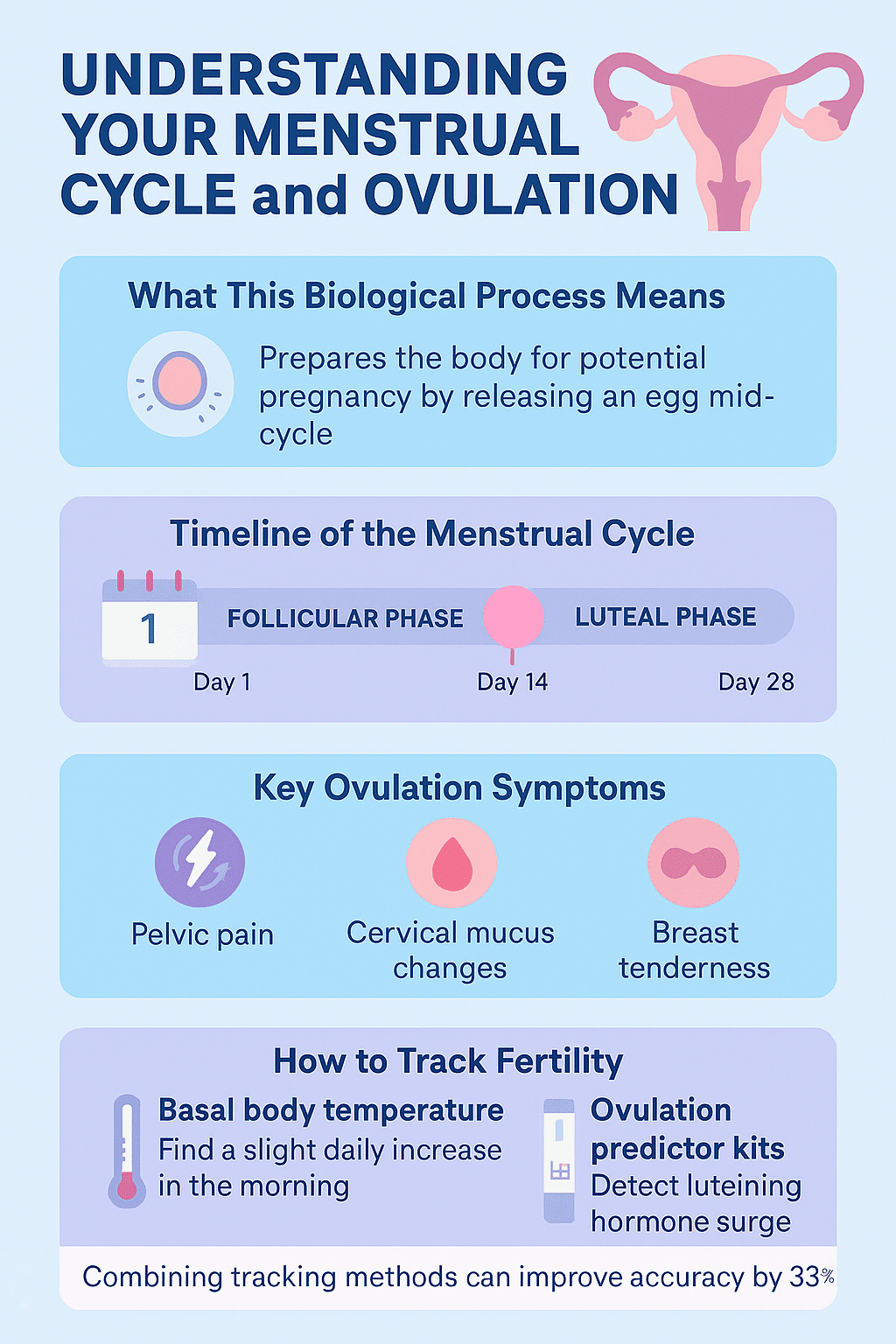
The menstrual cycle is a carefully orchestrated process involving key hormonal events. Over roughly 28 days, your body prepares for potential pregnancy through distinct phases. Medically reviewed guidelines confirm ovulation typically happens mid-cycle, when hormonal surges trigger egg release.
What This Biological Process Means
Ovulation marks the window when an egg leaves the ovary, ready for fertilization. Your uterine lining thickens simultaneously, creating ideal conditions for implantation. Recognizing these patterns helps pinpoint when conception is most likely.
Hormonal Drivers Behind the Scenes
A spike in luteinizing hormone (LH) acts as the primary trigger for egg release. Estrogen levels rise first, stimulating LH production. After ovulation, progesterone increases to support potential pregnancy. Tracking these hormonal shifts through symptoms ovulation predictors like cervical changes or mild cramping provides actionable insights.
Understanding your menstrual cycle’s rhythm transforms guesswork into strategy. By decoding these biological signals, you gain control over family planning decisions.
Timeline of Ovulation: From Menstruation to Mid-Cycle
Have you ever wondered how your body prepares for potential conception each month? The process begins on day one of your menstrual cycle, when bleeding starts. This marks the follicular phase – a critical period where hormones activate changes to support reproductive readiness.
The Follicular Phase Explained
During the first 13-14 days, follicles in your ovaries mature under hormonal guidance. One dominant follicle eventually releases an egg – typically around day 14 in standard cycles. This “day ovulation” event creates a 12-24 hour window for fertilization.
Insights into the Luteal Phase
After the egg releases, the luteal phase begins. Lasting approximately 14 days, this stage sees progesterone levels rise to thicken the uterine lining. If conception occurs, these changes support early pregnancy. If not, the cycle restarts.
Understanding this timeline helps predict your “day ovulation” with greater accuracy. While cycle lengths vary, the follicular and luteal phases work together to optimize your chances during each menstrual cycle.
Key Ovulation Symptoms You Should Know
Your body sends clear signals when fertility peaks. Physical changes act as nature’s alert system, offering clues about your reproductive window. Learning to interpret these markers turns subtle shifts into actionable data.
Recognizing Physical Signs
Mild pelvic discomfort often accompanies symptoms ovulation. This twinge – called mittelschmerz – typically lasts minutes to hours. About 20% of women notice this pain when the ovary releases an egg.
Breast tenderness and heightened senses may also occur. These changes stem from hormonal fluctuations preparing the body for potential conception. Tracking these patterns helps predict your most fertile phase.
Changes in Cervical Discharge
Cervical mucus transforms into a stretchy, egg whites-like texture during ovulation. This discharge creates pathways for sperm survival. Its clear, slippery consistency differs markedly from drier pre-ovulation phases.
Observing these variations requires daily checks. Fertile-quality mucus usually appears 1-2 days before pain signals. Combining both indicators boosts tracking accuracy.
Consistent monitoring turns biological cues into powerful planning tools. Documenting discharge changes and physical sensations builds reliable fertility forecasts over time.
Tracking Ovulation: Tools and Techniques
What tools turn cycle tracking into actionable insights? Reliable methods like basal body temperature monitoring and ovulation predictor kits bridge the gap between observation and results. These approaches detect subtle physiological shifts that reveal your most fertile days.
Methods to Monitor Your Basal Body Temperature
Your basal body temperature rises slightly after ovulation due to progesterone. A specialized thermometer detects changes as small as 0.4°F. Measure orally each morning before movement or talking.
Chart readings daily to spot patterns. Three consecutive higher temperatures confirm ovulation occurred. This method works best when combined with other tracking strategies for timing conception attempts.
Using Ovulation Predictor Kits
These kits detect luteinizing hormone (LH) surges in urine – the final trigger before egg release. Start testing 2-3 days before your expected fertile window. Positive results mean ovulation will likely occur within 24-36 hours.
For best accuracy, test at the same time daily. Pair kits with temperature tracking to confirm ovulation happened. When used consistently, these tools help you get pregnant by identifying prime conception opportunities.
Both methods require patience but offer clarity. Recording data reveals your unique patterns, turning guesswork into informed planning. Whether aiming to conceive or understand your cycle, these techniques provide science-backed guidance.
Ovulation Guide: Timeline, Symptoms, and How to Track Fertility
Precision matters when mapping your fertility patterns. Medically reviewed studies show combining tracking techniques improves prediction accuracy by 33% compared to single-method approaches. This multi-layered strategy helps pinpoint when ovulation happens with greater confidence.
Combining Methods for Greater Accuracy
Pair temperature charts with ovulation kits for cross-verified results. Basal body thermometers detect post-ovulation shifts, while test strips identify the LH surge preceding egg release. Time intercourse within 12 hours of a positive kit result for optimal chances.
Add cervical mucus observations to your toolkit. When stretchy discharge coincides with kit positives and temperature rises, you’ve likely found your fertile window. These overlapping signals create a biological confirmation system.
Interpreting Your Cycle Data Effectively
Look for patterns across 3+ cycles to account for natural variations. Note the time between LH surges and temperature spikes – this gap reveals how quickly ovulation happens after hormonal changes. Most medically reviewed guidelines suggest fertile days span 5-7 days monthly.
Use apps to visualize trends, but stay engaged with raw data. Sudden cycle shifts might indicate stress or health changes needing attention. Consistent tracking transforms scattered observations into actionable insights for conception planning.
Using Technology to Monitor Fertility
Modern tools transform how you understand your reproductive health. Mobile apps and wearable tech now offer real-time insights once only available in clinical settings. These innovations simplify fertility tracking while improving accuracy through automated data collection.
Cycle Tracking Apps and Software
Apps like Flo sync with wearables to log body temperature, sleep patterns, and cycle dates. They analyze trends across months to predict fertile windows. Instead of manual charts, these platforms send alerts when tracking ovulation becomes critical.
Wearable Devices and Smart Thermometers
Smart thermometers measure body temperature with 0.05°F precision overnight. Paired with rings or wristbands, they detect subtle shifts indicating hormonal changes. Data flows directly to apps, eliminating guesswork.
Continuous monitoring spots patterns you might miss. For example, a slight body temperature rise after exercise could affect readings. Tech accounts for these variables automatically.
Adopting these tools streamlines tracking ovulation while boosting confidence. They turn scattered observations into cohesive reports, empowering smarter decisions about your fertility journey.
Natural Methods for Confirming Ovulation
Your body broadcasts subtle signs when preparing for conception opportunities. While technology offers precision, biological cues provide accessible confirmation methods requiring no special equipment. Tuning into these natural indicators helps build a complete picture of your reproductive patterns.
Observing Physical Changes
Tracking basal body shifts manually can reveal critical patterns. Each morning before rising, check underarm temperature with a standard thermometer. Consistent rises of 0.5-1°F often follow egg release when recorded every day.
Cervical position changes offer another clue. During fertile phases, it becomes higher and softer. Combine these observations with mucus texture notes for cross-verification. Many people find this approach helps reduce reliance on devices.
Identifying Mittelschmerz and Other Cues
Mild pelvic twinges – mittelschmerz – affect 1 in 5 individuals during egg release. This brief discomfort often coincides with other signs like heightened energy levels or increased focus. Track these sensations every day alongside physical changes.
Breast sensitivity and appetite fluctuations may also emerge. While not universal, these biological signals help complete your fertility puzzle. Documenting them creates patterns that complement tech-based tracking methods.
Natural observation strengthens self-awareness while building reliable records. When combined with medical guidance, these techniques empower people to understand their unique basal body rhythms without overwhelming complexity.
Dealing with Irregular Ovulation
Cycle irregularities often leave more questions than answers. While occasional variations are normal, persistent changes might signal deeper health considerations. Understanding these patterns helps you distinguish between temporary fluctuations and potential red flags.
Identifying Underlying Causes
Stress, extreme diet changes, or conditions like PCOS can disrupt your cycle’s rhythm. Your reproductive tract relies on hormonal harmony – imbalances here may delay or prevent egg release. Track cycle lengths and symptoms for three months to spot concerning trends.
When to Seek Medical Advice
Consult a doctor if cycles are shorter than 21 days or exceed 35 days regularly. Missing periods for 90+ days or severe pelvic pain also warrant evaluation. These signs could indicate thyroid issues, insulin resistance, or structural abnormalities needing attention.
Proactive monitoring supports both conception goals and overall health. Simple steps like maintaining a cycle journal help identify patterns. Share these records with your doctor to streamline diagnosis and treatment options.
Your body’s signals matter. Addressing irregularities early preserves reproductive tract function and hormonal balance. Knowledge transforms uncertainty into empowered decisions for your wellness journey.
Optimizing Timing for Conception
What if perfect timing could be your greatest ally in conception? The fertile window – a 6-day period ending at ovulation – offers your best chance to get pregnant. Research shows 80% of pregnancies occur when intercourse happens during this critical phase.
Understanding Your Fertile Window
Your fertile window includes the 5 days before ovulation and the day of egg release. Sperm survive up to 5 days, while the egg lasts 12-24 hours. This overlap creates prime opportunities. Aim for sex every other day during this stretch, especially the 48 hours before ovulation.
Best Practices for Family Planning
Family planning succeeds when you align efforts with biological realities. Track cervical mucus changes and LH surges to pinpoint your window. Schedule intimacy when discharge resembles raw egg whites – nature’s green light for conception.
Consistency matters. Couples who have sex 2-3 times weekly during their fertile window triple their chances to get pregnant compared to sporadic attempts. Pair timing with ovulation kits for precision.
Proactive tracking transforms hope into strategy. By mastering your cycle’s rhythm, you turn six days of potential into powerful family planning results.
Medically Reviewed Guidelines and Expert Insights
Trusted medical guidance transforms fertility tracking from uncertainty to clarity. Leading gynecologists and reproductive specialists emphasize strategies validated through rigorous research. These medically reviewed approaches combine biological science with practical application for reliable results.
What Experts Recommend
Flo Health’s clinical advisors suggest pairing basal body temperature charts with ovulation predictor kits. This dual-method approach aligns with medically reviewed studies showing 76% accuracy in predicting fertile windows. Dr. Amanda Richards, a board-certified OB-GYN, notes: “Consistent tracking across three cycles reveals patterns technology alone might miss.”
Regular check-ins with your doctor help customize these methods. They can adjust your plan based on cycle irregularities or health history. Many clinics now use standardized fertility assessment tools developed through peer-reviewed trials.
Ensuring Accuracy Through Evidence-Based Methods
Clinical guidelines prioritize methods tested in controlled studies over anecdotal advice. For example, luteal phase tracking proves more reliable than calendar predictions alone. Research shows temperature spikes confirm ovulation occurred 89% of the time when measured correctly.
Documentation matters. Experts advise logging symptoms daily rather than relying on memory. Share these records during medical consultations to spot trends. Evidence-based tracking reduces guesswork while aligning with your body’s unique rhythms.
Conclusion
Mastering your cycle’s rhythm transforms uncertainty into actionable plans. By understanding menstrual cycle phases and tracking body temperature shifts, you gain control over conception timing. Methods like basal body temperature charts and ovulation kits pinpoint when the egg is released – critical data for planning.
Consistency across months matters most. Daily body temperature checks and recognizing fertile window patterns reveal your unique biological blueprint. While symptoms like mild pain or cervical changes offer clues, combining multiple tracking methods boosts accuracy.
Your reproductive tract holds answers – listen through disciplined observation. Trust medically reviewed strategies to optimize chances to get pregnant. If irregularities persist beyond three months, consult a specialist. Knowledge empowers every step of your journey.

