It’s one of those things you probably don’t think much about, until something feels… off. Maybe it’s a sharp pain in your side that wasn’t there before, or a worrying tinge of pink when you go to the bathroom. Our kidneys, those amazing little filters, work tirelessly day in and day out. When they run into trouble, it can be unsettling. One such problem, though not incredibly common, is something called Renal Papillary Necrosis.
Let’s talk about what that actually means.
Understanding Your Kidneys and Renal Papillary Necrosis
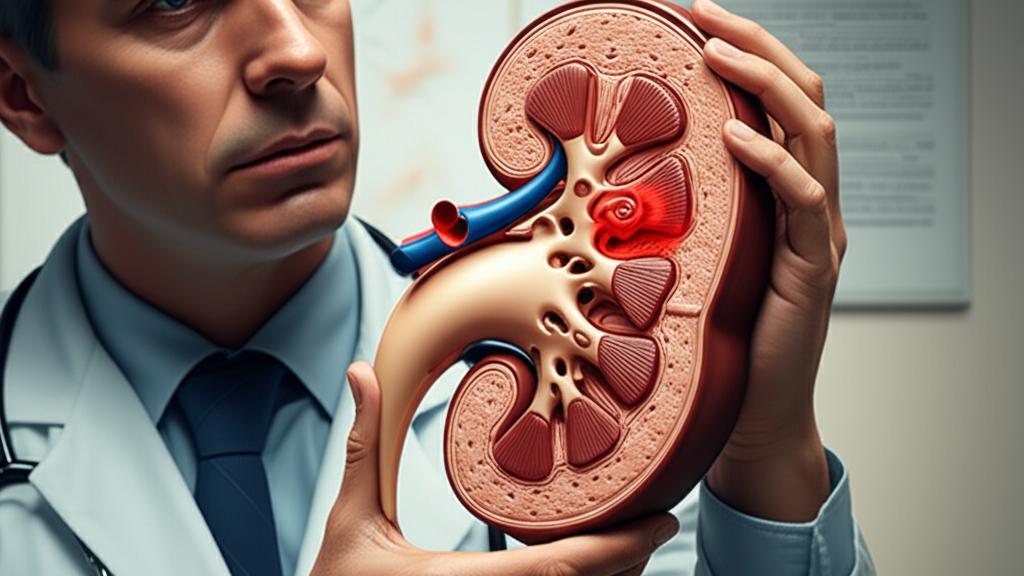
Think of your kidneys – most of us have two – as sophisticated cleaning stations for your blood. Blood flows into them through big vessels called renal arteries, which then branch out into tinier and tinier ones. In the outer part of your kidney, special cells grab waste products and extra water from your blood.
This watery waste, which we know as urine, then travels through a network of tiny tubes towards the center of your kidney, an area called the medulla. The medulla has these funnel-shaped bits of tissue. Inside each funnel, the tiny tubes empty into larger collecting ducts. The very tip of this funnel, where these ducts meet, is called the renal papilla. It’s a crucial spot.
From these renal papillae, urine moves into the central collecting area of your kidney. Then, it’s down the ureter (the tube connecting kidney to bladder), into your bladder, and finally out of your body through the urethra.
So, Renal Papillary Necrosis is when the cells and tissue in that middle region (the medulla) and specifically in the renal papillae die off. It’s like a part of the kidney’s drainage system gets damaged. When these areas of tissue die, it can reduce how well your kidneys work and, in serious cases, can even lead to kidney failure.
It tends to show up more often in folks over 60, and women seem to experience it a bit more commonly than men. Often, if it happens, it can affect both kidneys – in about 7 out of 10 people, that’s the case.
What Can Cause This Kidney Issue?
There isn’t just one culprit behind Renal Papillary Necrosis. Several conditions and factors can unfortunately lead to it. The most common ones we see are:
- Diabetes: This is a big one.
- Overdoing it with nonsteroidal anti-inflammatory drugs (NSAIDs) – think aspirin, ibuprofen, and naproxen. Using them too much or for too long can be hard on the kidneys.
- Sickle cell disease: A blood disorder that can affect many parts of the body, including the kidneys.
But those aren’t the only possibilities. Other conditions that might play a role include:
- Chronic liver disease
- Pyelonephritis (that’s a bacterial infection in your kidney)
- Renal tuberculosis (a type of TB that settles outside the lungs, in the kidney)
- Renal vein thrombosis (a blood clot in the vein that takes blood away from your kidney)
- Ureteral obstruction (a blockage in that tube, the ureter)
- Vasculitis (which is inflammation of your blood vessels)
Spotting the Signs of Renal Papillary Necrosis
Here’s the tricky part: in the early stages, you might not notice anything at all. Zero symptoms. This can make it tough to catch Renal Papillary Necrosis early on. Sometimes, we stumble upon it when we’re looking into or treating one of the underlying conditions I just mentioned.
But as it gets more advanced, you might start to experience:
- Dysuria: That’s a medical term for painful urination. Ouch.
- Fever and chills: Feeling like you’ve got the flu, but it could be your kidneys.
- Hematuria: This means blood in your urine. Sometimes you can see it (it might look pink, red, or cola-colored), other times it’s only visible under a microscope.
- Nocturia: Having to get up to pee frequently during the night.
- Pyuria: An unusually high number of white blood cells in your urine, which often signals an infection or inflammation.
- Severe flank pain: A sharp, intense pain on one or both sides of your back, kind of between your ribs and hips.
- Urinary tract infections (UTIs): These can sometimes be a sign of deeper kidney trouble.
How We Figure Out What’s Going On: Diagnosis
If you come to the clinic with some of these symptoms, or if we suspect something might be up with your kidneys due to another health condition, we’ll need to do some investigating. To diagnose Renal Papillary Necrosis, we often use a few key tools:
- Urography: This involves getting pictures of your kidneys. It could be an X-ray, CT scan, or MRI. Before the scan, you’d get an intravenous (IV) dye, called contrast. This special dye helps us see any damaged areas in your kidneys much more clearly on the images.
- Ureteroscopy: This sounds a bit intense, but it’s a way for us to get a direct look inside your kidneys. We use a very thin, flexible tube that has a tiny camera on the end.
- Kidney biopsy: Sometimes, the best way to know for sure is to take a very small sample of kidney tissue. A specialist called a pathologist (a doctor who studies tissues and cells) then looks at it under a microscope to see what’s happening at a cellular level.
Blood and Urine Tests: The Kidney Detectives
Blood and urine tests are also super important. They give us clues about how well your kidneys are doing their filtering job. These might include:
- Blood urea nitrogen (BUN): This test measures nitrogen in your blood. If your kidneys aren’t filtering well, BUN levels can go up.
- Creatinine: This is a waste product from normal muscle wear and tear. Your kidneys usually clear it out. Higher creatinine levels can also point to kidneys not working at their best.
- Estimated glomerular filtration rate (eGFR): This isn’t a direct measurement but a calculation. We use your blood protein levels, creatinine, age, sex, size, and race to estimate how well your kidneys are filtering blood.
- Urinalysis: This is a good look at your urine – visually, under a microscope, and with chemical tests. We can spot blood (both red and white blood cells). Sometimes, with Renal Papillary Necrosis, we can even see tiny broken-off pieces of the renal papillae in the urine under the microscope.
- Urine protein/creatinine ratio: Finding protein in your urine (where it normally shouldn’t be much) is often a sign of kidney damage.
What Happens if Renal Papillary Necrosis Isn’t Treated?
It’s really important to catch and manage this condition. If left untreated, Renal Papillary Necrosis can lead to some serious problems, like:
- Chronic kidney disease (CKD)
- Kidney failure (where your kidneys can no longer do their job)
- Needing dialysis (a machine to clean your blood)
- Potentially needing a kidney transplant
There’s also an association between Renal Papillary Necrosis and a type of cancer called transitional cell cancer, which can occur in the kidney or ureter.
How We Approach Treatment
Now, for the treatment part. There isn’t one specific pill or procedure that directly “fixes” Renal Papillary Necrosis itself. Instead, our main goal is to manage the underlying cause – whatever that might be from the list we talked about earlier. By treating the root problem, we aim to stop any more damage to your kidneys.
How well treatment works really depends on how much damage has already been done. In more severe cases, even with treatment, the kidney damage might continue to progress. But in less severe situations, we can sometimes stabilize kidney function, or it might even get a bit better. We’ll discuss all the options available for you.
Looking Ahead: What’s the Outlook?
Your outlook, or prognosis, really hinges on what caused the Renal Papillary Necrosis and how extensive the damage is. For instance, folks with diabetes often face a tougher road because diabetes is a long-term condition that isn’t always easy to keep perfectly controlled. If you have diabetes, doing your very best to manage it is key to protecting your kidneys.
Severe Renal Papillary Necrosis can be quite serious, potentially leading to dialysis or a kidney transplant. If infections develop, it can even be life-threatening. Sadly, death can also occur from kidney failure.
In conditions like sickle cell disease, Renal Papillary Necrosis is one of several kidney complications that can arise. Taken together, these can unfortunately reduce a person’s life expectancy.
Can We Prevent Renal Papillary Necrosis?
Prevention is always the best medicine, right? You can take steps to reduce your risk:
- Focus on good overall health.
- If you use NSAIDs (like ibuprofen or naproxen) or other over-the-counter pain relievers, always use them according to the instructions on the label or as your doctor advised. Don’t take more than recommended or for longer than you should.
- If you have a condition like diabetes, sickle cell disease, or any other illness that can cause Renal Papillary Necrosis, it’s so important to follow your healthcare provider’s care plan closely. Attend your regular appointments. You’ll likely need routine lab tests to keep an eye on your kidney function and catch any changes early.
Take-Home Message: Key Points on Renal Papillary Necrosis
Alright, let’s boil this down to the essentials:
- Renal Papillary Necrosis is damage and death of tissue in a specific part of your kidney called the renal papillae.
- Common causes include diabetes, overuse of NSAID pain relievers, and sickle cell disease.
- Symptoms might not appear early, but can include flank pain, blood in urine, painful urination, and fever/chills.
- Diagnosis involves imaging (like CT scans with contrast), looking inside with a scope, and blood/urine tests to check kidney function.
- Treatment focuses on managing the underlying condition causing the Renal Papillary Necrosis.
- Prevention involves managing risk factors and any existing health conditions carefully.
When to Reach Out to Your Doctor
Please don’t hesitate to get in touch with your doctor or our clinic if you experience any of these:
- Seeing blood in your urine.
- Running a fever or having chills that you can’t explain.
- Pain when you urinate.
- Pain on either side of your back, tucked in between your hip bones and your ribs.
It’s always better to get things checked out. We’re here to help you figure out what’s going on and get you the care you need. You’re not alone in this.