Imagine your body has this super smart internal control system, always working behind the scenes to keep things balanced. One of the unsung heroes in this system, especially when it comes to your blood pressure, is something called renin. You might hear about it if we’re trying to figure out why your blood pressure is a bit stubborn, or if certain medications aren’t quite doing the trick. It’s a tiny enzyme, but boy, does it have a big job.
What is Renin, Anyway?
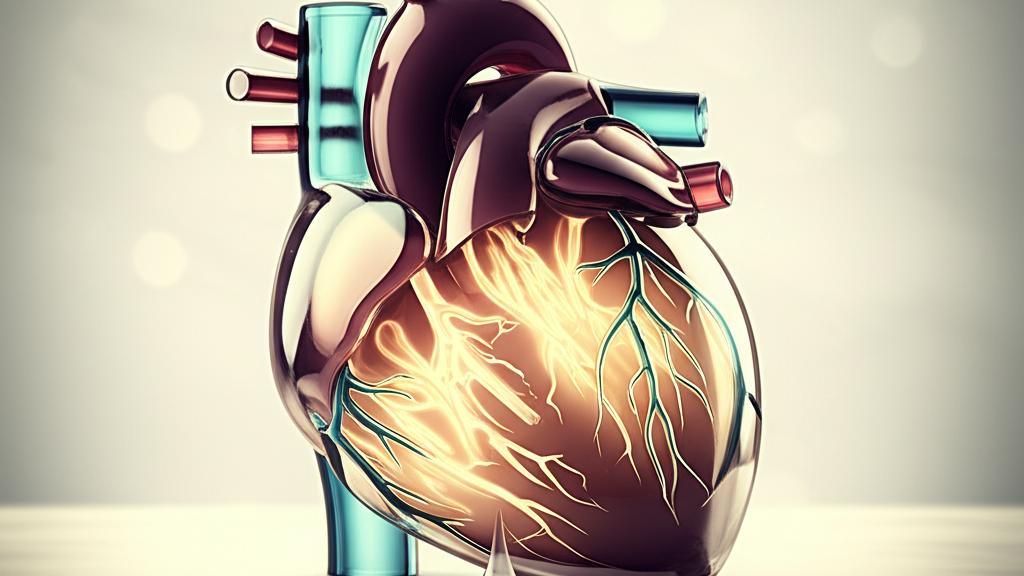
So, what exactly is renin? Well, it’s an enzyme – think of enzymes as little helpers that speed up chemical reactions in your body. This particular helper is made by special cells in your kidneys. Renin is a key player in a chain reaction called the renin-angiotensin-aldosterone system, or RAAS for short. It’s a bit of a mouthful, I know! But essentially, this system is designed to keep your blood pressure just right. Specifically, renin kicks off the process that controls the production of another important substance, a hormone called aldosterone, which is made by your adrenal glands (those little glands sitting on top of your kidneys).
The Body’s Balancing Act: How Renin Steps In
The main job of renin is to help regulate your blood pressure. It doesn’t do this alone; it’s part of a team with angiotensin (another hormone) and aldosterone. Together, they fine-tune the levels of sodium and potassium in your body, which in turn affects your fluid balance and blood pressure.
Here’s a simplified look at how it all connects:
- When your body needs to raise blood pressure, renin gets to work. It converts a protein made by your liver, called angiotensinogen, into something called angiotensin I.
- Then, angiotensin I gets changed into angiotensin II.
- Now, angiotensin II is the real mover and shaker here. It does two main things: it narrows your blood vessels (which naturally raises pressure), and it tells your adrenal glands to release aldosterone.
- Aldosterone then signals your kidneys to hold onto salt and water. More fluid in your system means… you guessed it, increased blood pressure. See? It’s like a carefully orchestrated dance.
So, when does renin get the signal to jump into action? Your body is pretty clever about this. Renin is released into your bloodstream when:
- Your blood pressure dips too low. Special sensors in your arteries, called baroreceptors, pick up on this.
- Your kidneys sense that your salt (sodium) levels are too low.
- There’s activity in your sympathetic nervous system – that’s your ‘fight or flight’ system. Certain receptors, known as beta 1 adrenergic receptors (which also help regulate your heart rate), can trigger renin release.
It’s important to remember that renin itself doesn’t directly jack up your blood pressure. It’s the conductor of the orchestra, setting off the chain of events that leads to angiotensin II and aldosterone doing their jobs.
As I mentioned, your kidneys are the production house for renin. When your systolic blood pressure (the top number in your BP reading) drops, or if your kidneys sense you’re low on fluids (what we call volume depleted), they release renin into your bloodstream to get that balancing act started.
Highs and Lows: What Do Your Renin Levels Mean?
Sometimes, this finely tuned system can get out of whack, and renin levels can be too high or too low. This can give us clues about what might be going on with your health.
What if Your Renin is High?
If a blood test shows high renin levels, it could be your body’s appropriate response to something, or it might point to an underlying issue. We might see high renin with:
- Hypotension (that’s low blood pressure).
- Significant blood loss or hemorrhage.
- Reduced blood flow to your kidneys.
- Dehydration or other causes of volume depletion (not enough fluid in your system).
- Increased sympathetic nerve activation (like during stress or with certain conditions).
- Addison’s disease, a condition where your adrenal glands don’t make enough hormones, especially if it’s causing volume depletion.
- Low potassium levels in your blood (hypokalemia).
- Rarely, renin-producing kidney tumors.
- Renal hypertension, which is high blood pressure specifically caused by narrowed arteries leading to your kidneys.
- Malignant hypertension – this is a very high, sudden-onset blood pressure.
- Sometimes, even with primary hypertension (the common type of high blood pressure with no single identifiable cause).
- In conditions like heart failure or cirrhosis (scarring of the liver), if they lead to what we call low effective blood volume, even if you have fluid overload elsewhere. It’s a bit complex, that one.
And If Your Renin is Low?
On the flip side, low renin levels can also tell us a story. This might happen with:
- Primary aldosteronism (PA), also known as Conn’s syndrome. This is a key one. Here, your adrenal glands are making too much aldosterone on their own, so the body tries to shut down renin production.
- Certain steroid therapies that cause your body to retain salt.
- Salt-sensitive hypertension, where high blood pressure is particularly reactive to how much salt you eat.
Checking Your Renin: The ‘Why’ and ‘How’
If we’re trying to get to the bottom of tricky high blood pressure, especially if the usual medications aren’t working as well as we’d like, we might suggest a renin test. Often, we’ll test it alongside your aldosterone level. This combination helps us see how much aldosterone your adrenal glands are actually making and if the RAAS system is balanced.
This is particularly useful if we suspect primary aldosteronism (PA). People with PA often have high blood pressure that’s tough to control because their bodies are making too much aldosterone. The renin and aldosterone tests together can help confirm or rule this out.
How do we measure it? Most commonly, we measure something called plasma renin activity (PRA). This test looks at how well your renin is doing its job of starting the process to make angiotensin I. Sometimes, we might measure direct renin levels too. It’s a simple blood test, usually.
Keeping Your Renin System in Balance
If your renin levels are off – either too high or too low – the approach really depends on why. We don’t treat the renin number itself; we treat the underlying cause.
For example, if you have high renin and high blood pressure, and we’ve ruled out things like primary aldosteronism, there are medications that can help. These might include:
- Beta-blockers
- Clonidine
- Other types of blood pressure medications that can influence the RAAS system.
But again, it’s all about figuring out the root of the issue. We’ll always discuss all the options and what they mean for you.
Key Things to Remember About Renin
Alright, that was a lot of information, I know! Here are the main things I hope you’ll take away about renin:
- Renin is a vital enzyme made by your kidneys.
- It’s a crucial part of the renin-angiotensin-aldosterone system (RAAS), which helps regulate your blood pressure.
- Renin kicks off a chain reaction that leads to the production of aldosterone and the narrowing of blood vessels, ultimately affecting fluid balance and blood pressure.
- Levels can be too high or too low due to various conditions, from dehydration to more specific disorders like primary aldosteronism.
- A renin test, often done with an aldosterone test, can help us understand the cause of hard-to-treat high blood pressure.
- Treatment focuses on the underlying cause of abnormal renin levels, not just the number itself.
So, while renin might be a term you don’t hear every day, it’s a hardworking little molecule doing a big job. If it ever comes up in our conversations, now you’ll have a better idea of what we’re looking into. And remember, we’re in this together to figure things out.