Ever heard of ringworm and pictured tiny worms? Despite its name, ringworm has nothing to do with worms! It’s actually a very common type of fungal skin infection, medically known as tinea. When certain fungi decide to set up camp on your skin, they can cause rashes that, while usually mild, can be quite annoying and itchy.
Think of it like this: different types of tinea infections get different names depending on where they show up on your body. You’ve probably heard of some of them:
- Jock Itch (Tinea Cruris): When the fungus grows in the groin, upper thighs, or buttocks area.
- Athlete’s Foot (Tinea Pedis): When it affects the feet.
- Ringworm (Tinea Corporis / Tinea Capitis): When this type of fungus appears elsewhere on the body, it’s generally called ringworm. Specifically, it’s tinea corporis on the body skin and tinea capitis when it’s on the scalp.
- Nail Fungus (Onychomycosis or Tinea Unguium): When the infection settles into fingernails or toenails.
No matter the name, the culprit is usually a similar type of fungus.
💡 Key Takeaway: Ringworm = Fungal Infection (Tinea), NOT a worm! Different names apply depending on the body part affected.
What Does Ringworm Look and Feel Like? (Signs & Symptoms)
So, how do you know if you might have this common fungal rash? Symptoms vary depending on the location:
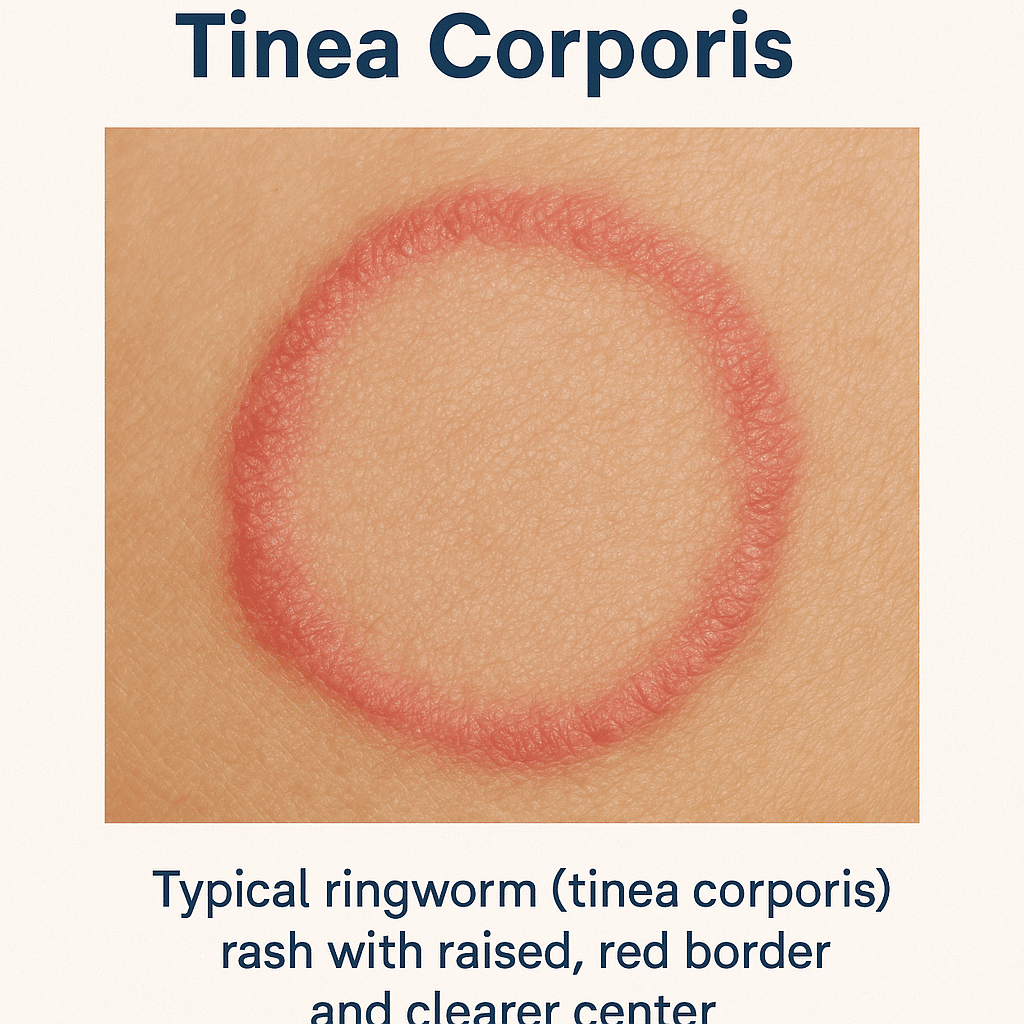
Ringworm Symptoms on the Skin (Tinea Corporis)
- Often starts as a red, scaly patch or bump.
- May develop into the classic “ring” shape: A circular rash with raised, bumpy, or scaly borders. The center might look clearer or less red. (But remember, not everyone gets the distinct ring!)
- The affected skin can flake, peel, or crack.
- Itchiness is very common. You might also feel stinging, burning, or general discomfort in the area.
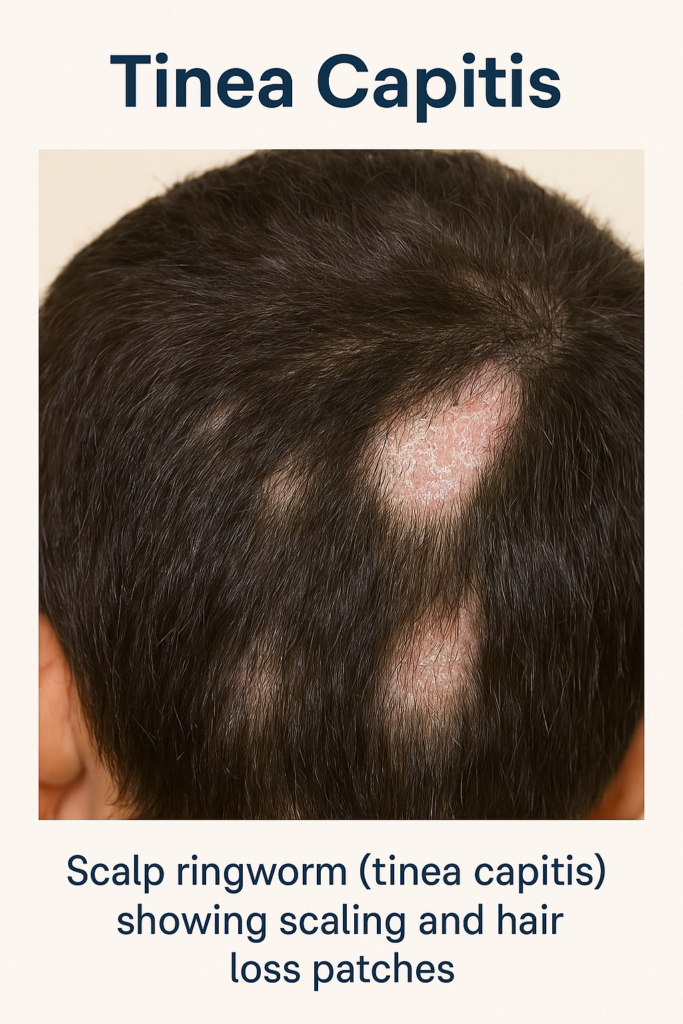
Ringworm Symptoms on the Scalp (Tinea Capitis)
- Can begin as a small sore resembling a pimple.
- Often progresses to patchy, flaky, or scaly areas, sometimes looking like stubborn dandruff.
- May cause hair to fall out or break off near the scalp, sometimes leaving bald patches.
- The scalp might become swollen, tender, and red.
- Occasionally, a more severe, pus-filled, boggy swelling called a kerion can form.
- You might notice swollen lymph nodes (glands) at the back of the head or neck.
Ringworm Symptoms on the Nails (Onychomycosis / Tinea Unguium)
- Can affect one or multiple fingernails or toenails.
- Infected nails often become thick, brittle (crumbly), and discolored (usually white or yellowish).
What Causes This Fungal Rash?
Ringworm isn’t caused by poor hygiene! It’s caused by common types of fungi called Dermatophytes (pronounced: der-MAH-tuh-fites). These tiny organisms naturally live in small amounts on people’s skin, hair, and nails without causing problems.
However, when the conditions are right – typically warm and moist environments – these fungi can multiply rapidly, overgrow, and lead to the symptoms we recognize as ringworm, athlete’s foot, or jock itch.
Is Ringworm Contagious? How Does It Spread?
Yes, ringworm is contagious. This fungal infection can spread quite easily in several ways:
- Person-to-Person: Through direct skin-to-skin contact with someone who has the infection. Warm, damp environments make transmission easier.
- Self-Spread: If you touch an infected area on your body and then touch another part (like your hands, groin, or feet), you can spread the fungus.
- Animal-to-Person: You can catch ringworm from infected animals, most commonly pets like cats and dogs, but also rodents or farm animals.
- Object-to-Person: The fungi can survive on contaminated objects. Sharing items like combs, brushes, hats, towels, bedding, or clothing with an infected person can spread it.
- Environment-to-Person: Dermatophytes thrive in warm, damp places like public showers, locker room floors, and pool surrounds. Walking barefoot in these areas increases your risk.
Close physical contact, like in sports such as wrestling, also makes spreading easier.
Who Is More Likely to Get Ringworm?
While anyone can get ringworm, certain factors can increase your chances:
- Having minor skin injuries, like scratches or cuts (gives the fungus an entry point).
- Living in or frequently being exposed to warm, humid environments.
- Sweating heavily.
- Participating in contact sports.
- Using public showers or locker rooms frequently.
- Sharing personal items like towels or clothing.
- Having certain health conditions that may weaken the immune system, such as diabetes or obesity.
How Do Doctors Diagnose Ringworm?
Often, a doctor can diagnose ringworm simply by looking closely at the rash and asking about your symptoms, recent activities, and lifestyle. The characteristic appearance, especially the ring shape, is often a key clue.
Sometimes, to be certain it’s a fungal infection and not another skin condition, the doctor might perform a simple, painless test:
- Skin Scraping: Gently scraping a small sample of the affected skin flakes onto a slide.
- Microscope Exam (KOH Test): Looking at the sample under a microscope to check for fungal elements.
- Fungal Culture: Sending the sample to a lab to grow and identify the specific fungus (takes longer).
Getting Rid of Ringworm: Treatment Options
The good news is that ringworm is usually treatable! The approach depends on where the infection is and how severe it is:
- Mild Skin Infections (Tinea Corporis): Often respond well to over-the-counter (OTC) antifungal creams, sprays, or powders. Look for ingredients like clotrimazole, miconazole, terbinafine, or ketoconazole. Follow the package directions carefully.
- More Serious Skin Infections: May require stronger prescription antifungal medications, either topical (applied to the skin) or sometimes oral (pills/syrup), prescribed by your doctor.
- Scalp Ringworm (Tinea Capitis) & Nail Fungus (Onychomycosis): These usually need prescription oral antifungal medicine taken for 1 to 3 months to effectively reach the hair follicles or nail bed. Your doctor might also recommend using a prescription antifungal shampoo for scalp ringworm to help reduce shedding of fungal spores and prevent spreading.
Important Treatment Tips:
- Complete the Full Course: Use the antifungal medicine for the entire duration recommended by your doctor or the product label, even if the rash starts looking better. Stopping early is a common reason the infection comes back.
- Keep the Area Clean and Dry: Wash the affected area daily and dry it thoroughly with a separate, clean towel. Don’t use the same towel on other parts of your body.
- Apply Medicine as Directed: Follow instructions precisely.
- Change Clothes Daily: Especially underwear and socks if you have jock itch or athlete’s foot.
- Treat Other Fungal Infections: If you have athlete’s foot and ringworm elsewhere, treat both simultaneously to prevent re-infection.
How Long Does Treatment Take?
Most mild skin ringworm cases clear up within 2 to 4 weeks with consistent treatment. However, more stubborn infections, or those affecting the scalp or nails, can take up to 3 months of treatment (often with oral medication) to fully resolve. Be patient and persistent!
Preventing Ringworm: Tips to Lower Your Risk
While you can’t always prevent ringworm entirely, you can definitely reduce your risk by taking some preventative steps: (Source: CDC Prevention Info)
- Practice Good Hygiene: Wash your skin daily and dry yourself completely, especially after showering, swimming, or any sweaty activity. Pay attention to skin folds.
- Keep Personal Items Personal: Avoid sharing towels, clothing, combs, brushes, hats, or sports gear.
- Wash Thoroughly: Launder workout clothes, sports uniforms, towels, and bedding regularly.
- Choose Breathable Clothing: Avoid tight-fitting clothes that trap moisture, especially in warm weather. Opt for cotton or moisture-wicking fabrics.
- Change Daily: Put on fresh clothes, socks, and underwear every day.
- Protect Your Feet: Wear waterproof sandals or shower shoes in public showers, locker rooms, and pool areas.
[Internal Link Suggestion: Link to Athlete's Foot Prevention tips] - Wash Hands After Pet Contact: If you play with pets, wash your hands well afterward, especially if you notice any patchy hair loss on your animal (a possible sign of ringworm – get them checked by a vet!).
- Treat Other Fungal Infections Promptly: Address athlete’s foot or jock itch quickly to prevent spreading.
By taking these simple precautions, you can significantly lower your chances of dealing with this annoying, but treatable, fungal infection.
Frequently Asked Questions about Ringworm
What is the cause of ringworm?
Ringworm is caused by common fungi called dermatophytes. These fungi naturally live on skin, hair, and nails but can overgrow and cause infection in warm, moist conditions.
Does ringworm go away by itself?
While very mild cases might possibly fade over time, treatment with antifungal medication is usually recommended to fully clear the infection and prevent it from coming back or spreading to other areas or people. It often does not resolve completely on its own without treatment.
Is ringworm a serious problem?
Ringworm on the skin is generally considered a mild but annoying infection. However, infections on the scalp (tinea capitis) or nails (onychomycosis) can be more persistent and require longer treatment with prescription medication. Severe scalp infections can occasionally lead to complications like significant hair loss or a kerion (a boggy, inflamed sore). Prompt treatment helps avoid complications and spreading.
What attracts ringworm? / What factors increase risk?
The fungi causing ringworm thrive in warm, damp environments. Factors increasing your risk include direct skin contact with an infected person or animal (like cats or dogs), sharing contaminated personal items (towels, combs, clothing), frequenting damp public places (locker rooms, showers, pools), having minor skin scrapes or cuts, excessive sweating, wearing tight clothing, or having certain conditions like diabetes or a weakened immune system.
How to avoid ringworm?
Key prevention steps include keeping your skin clean and thoroughly dry, avoiding sharing personal items like towels and clothing, wearing footwear in public showers and locker rooms, changing clothes daily (especially after sweating), washing hands after touching pets, and promptly treating other fungal infections like athlete’s foot.


