Have you experienced discomfort or pain in your pelvic or genital area that you might describe as “sperm cramps”? While “sperm cramps” isn’t an official medical diagnosis (sperm cells themselves cannot cramp), the term often refers to very real pain or cramping sensations felt in the testicles, groin, perineum (the area between the scrotum and anus), or lower abdomen, sometimes related to ejaculation or sexual activity.
If you’re searching for information on “sperm cramps,” you’re likely trying to understand the cause of this discomfort. This article explores potential underlying medical conditions that could cause these symptoms. Understanding these actual possible causes is the first step toward finding relief.
Where Does Male Pelvic and Genital Pain Come From?
The pain you might be describing could originate from several structures within the male reproductive and urinary systems, located in the pelvis and groin, including:
- Prostate Gland: Involved in semen production.
- Testicles & Epididymis: Where sperm are made and stored.
- Vas Deferens & Seminal Vesicles: Tubes and glands involved in semen transport and production.
- Urethra: The tube carrying urine and semen.
- Pelvic Floor Muscles: Supporting muscles in the pelvis.
- Associated Nerves and Blood Vessels.
Inflammation, infection, muscle tension, nerve irritation, or structural issues in these areas can all lead to pain.
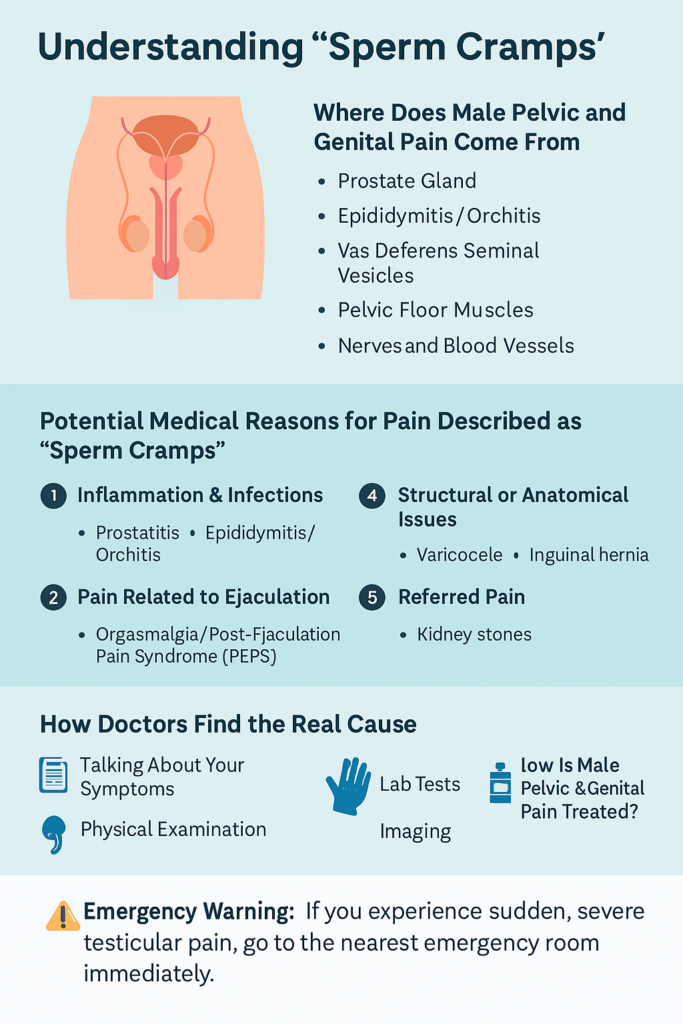
Potential Medical Reasons for Pain Described as “Sperm Cramps”
Here’s a look at established medical conditions that might cause the symptoms you’re experiencing:
1. Inflammation & Infections (Common Culprits)
- Prostatitis: This inflammation of the prostate gland is a frequent cause of pelvic pain in men under 50. It doesn’t always involve infection.
- Symptoms: Can include pain or aching in the perineum (between scrotum and anus), lower back, penis, or testicles; painful ejaculation (orgasmalgia); urinary urgency or frequency; sometimes a deep, hard-to-localize ache or cramping feeling.
- Causes: Can be bacterial (acute or chronic) or non-bacterial (Chronic Prostatitis/Chronic Pelvic Pain Syndrome – CP/CPPS), often involving inflammation without clear infection.
- Epididymitis / Orchitis: Inflammation of the epididymis (the sperm-carrying tube behind the testicle) or the testicle itself (orchitis). Often occur together (epididymo-orchitis).
- Symptoms: Testicular pain (ranging from dull ache to sharp, intense pain), scrotal swelling, redness, tenderness; sometimes fever or painful urination/ejaculation.
- Causes: Often bacterial infections, including STIs like chlamydia and gonorrhea in younger men, or urinary tract infections in older men, according to the Mayo Clinic.
2. Pain Related to Ejaculation
- Orgasmalgia / Post-Ejaculation Pain Syndrome (PEPS): Pain occurring specifically during or immediately after ejaculation. It can be felt in various pelvic/genital locations and might be sharp or cramp-like. This is often linked to underlying prostatitis or pelvic floor muscle issues.
3. Muscle-Related Pain
- Pelvic Floor Muscle Dysfunction: Chronic tension, tightness, or spasms in the pelvic floor muscles can cause a variety of symptoms, including deep pelvic ache, testicular pain, pain with ejaculation, urinary problems, and constipation. This pain can certainly feel like cramping. It can be related to stress, injury, posture, or other factors.
4. Structural or Anatomical Issues
- Varicocele: Enlargement of veins in the scrotum (like varicose veins). Can cause a dull ache, dragging sensation, or sometimes sharper pain, potentially perceived as cramping, especially after standing for long periods or physical exertion.
- Inguinal Hernia: When tissue protrudes through a weak spot in the abdominal muscles near the groin. Can cause pain or discomfort in the groin, sometimes radiating towards the testicles.
5. Referred Pain
- Kidney Stones: While originating in the kidney, the intense pain from a kidney stone moving through the urinary tract can radiate strongly to the groin and testicles.
6. Post-Surgical Pain
- Post-Vasectomy Pain Syndrome (PVPS): A small percentage of men experience chronic testicular or pelvic pain following a vasectomy.
7. URGENT: Testicular Torsion
- THIS IS A MEDICAL EMERGENCY. It happens when the testicle twists on its spermatic cord, cutting off blood supply.
- Symptoms: Sudden, severe, one-sided testicular pain, scrotal swelling, nausea/vomiting, abdominal pain.
- Action: Requires immediate emergency room visit. Treatment within hours is crucial to save the testicle. Learn more about Testicular Torsion from the Urology Care Foundation.
⚠️ Emergency Warning: If you experience sudden, severe testicular pain, go to the nearest emergency room immediately. It could be testicular torsion
What About “Sperm Buildup”?
You might read online about “sperm buildup” or “blue balls” (epididymal hypertension) causing pain from prolonged sexual arousal without ejaculation. While this can cause temporary aching or heaviness for some, it’s generally considered a temporary discomfort that resolves on its own and is distinct from the persistent, often more severe pain associated with the medical conditions listed above, which require evaluation. If you have recurring or significant pain, it’s unlikely to be simply “sperm buildup.”
How Doctors Find the Real Cause
Since “sperm cramps” isn’t a diagnosis, your doctor will focus on identifying the actual underlying condition causing your symptoms. The diagnostic process usually involves:
- Talking About Your Symptoms: A detailed discussion of the pain (location, type, severity, timing, triggers like ejaculation), your sexual health, urinary function, and overall medical history.
- Physical Examination: Including the abdomen, groin, genitals (penis, scrotum, testicles). A digital rectal exam (DRE) might be done to check the prostate.
- Lab Tests:
- Urine tests (urinalysis, urine culture) to look for infection or inflammation.
- STI testing (important if epididymitis or prostatitis is suspected).
- Possibly blood tests or semen analysis.
- Imaging: A scrotal ultrasound is often used to visualize the testicles, epididymis, and blood flow (crucial for ruling out torsion and diagnosing epididymitis or varicoceles). Imaging of the kidneys or pelvis might be needed in some cases.
- Specialist Referral: Often, a referral to a urologist is necessary for specialized diagnosis and treatment.
How Is Male Pelvic & Genital Pain Treated?
Treatment entirely depends on the identified underlying cause:
- Antibiotics: For bacterial infections like bacterial prostatitis or epididymitis.
- Anti-inflammatory Drugs (NSAIDs): Like ibuprofen or naproxen to reduce pain and inflammation.
- Pain Relievers: Over-the-counter or prescription options.
- Alpha-blockers: Medications to relax muscles in the prostate and bladder neck, often used for prostatitis/CPPS or BPH-related symptoms.
- Pelvic Floor Physical Therapy: Highly effective for pelvic floor dysfunction, teaching relaxation and control exercises.
- Lifestyle Adjustments: Warm baths, stress management, dietary changes (for some types of prostatitis).
- Surgery: Required urgently for testicular torsion, and sometimes elected for problematic varicoceles or hernias.
When Should You See a Doctor?
Don’t ignore persistent or severe pain in the pelvic or genital area.
- Go to the Emergency Room Immediately If: You experience sudden, severe testicular pain.
- Make a Doctor’s Appointment Promptly If:
- Pain is persistent, recurring, or worsening.
- You have pain accompanied by fever or chills.
- You notice swelling, redness, lumps, or changes in your scrotum/testicles.
- You experience painful urination, urinary frequency/urgency, or blood in urine/semen.
- You have discharge from your penis.
- Ejaculation is consistently painful.
Moving Beyond “Sperm Cramps”
While “sperm cramps” might be how you initially describe your discomfort, understanding that this term points towards potential underlying medical conditions is key. Pain in the male pelvic and genital region has various possible causes, from treatable infections and inflammations to muscle dysfunction or, rarely, emergencies.
Getting an accurate diagnosis from a healthcare professional is crucial for effective treatment and relief. If you’re experiencing concerning symptoms, reach out to your doctor or a urologist for proper evaluation and care.


