The early morning sunlight filtered through the clinic’s curtains, casting soft patterns on the walls. The gentle hum of the air conditioner blended with the faint rustling of papers and the occasional chime of the bell at the entrance. I was reviewing the day’s appointments when the door swung open, and Meera walked in, cradling her baby boy, Aarav. She gave me a weary smile, her eyes lined with fatigue.
“Good morning, Dr. Priya,” she said, adjusting Aarav in her arms. His round, bright eyes peeked out from beneath a blue beanie, but I noticed that his right eye was glossy, with a small streak of dried discharge near the corner.
I returned her smile warmly. “Good morning, Meera. What seems to be bothering Aarav today?”
She sighed and sat down across from me. “It’s his eye, Priya. It’s been watery for weeks now. Some mornings, it’s crusted shut with this yellowish gunk. I clean it, but it just keeps happening.”
I leaned in to get a closer look at Aarav. His right eye, though not red or swollen, glistened with tears that didn’t seem to drain away. The tell-tale signs of a blocked tear duct were clear.
What Is Tear Duct Blockage?
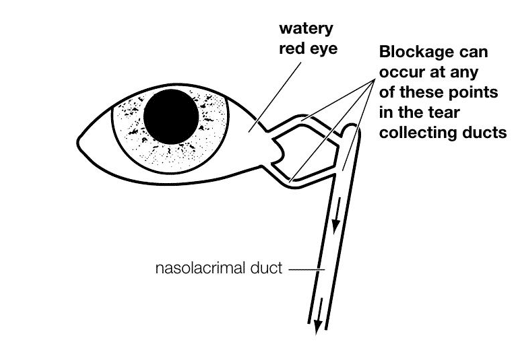
I gently stroked Aarav’s chubby hand as I explained. “Meera, what Aarav is experiencing is a common condition called a blocked tear duct, or nasolacrimal duct obstruction. It happens when the small ducts that drain tears from the eyes to the nose are not fully open.”
I continued, “Normally, tears flow through these ducts into the nose. But if the ducts are blocked, the tears have nowhere to go. This leads to watery eyes and sometimes, like in Aarav’s case, a bit of sticky discharge.”
Meera nodded, concern etched on her face. “Will it go away on its own?”
Why Does It Happen?
I reassured her. “Most of the time, yes. In infants, this happens because the ducts are still developing. It’s very common, affecting up to 5% of newborns. The blockage usually becomes noticeable between 3 and 12 weeks of age. It can affect one eye or both.”
I paused, giving Aarav a playful tickle, earning a tiny giggle from him. “It’s not something you did wrong, Meera. It’s just part of how some babies develop.”
Symptoms to Watch For
I listed the typical symptoms of tear duct blockage, pointing to Aarav’s eye as an example:
- Excessive tearing or watery eyes, even when the baby isn’t crying.
- Sticky or yellow discharge, especially noticeable after naps or in the morning.
- Crusting on the eyelids due to dried tears or discharge.
- Redness around the inner corner of the eye, though the white part of the eye remains clear.
- Swelling or tenderness if an infection develops.
Meera sighed. “Yes, every morning I find his eye stuck shut with crust. I feel so bad when he wakes up like that.”
Risks of Tear Duct Blockage
I gently touched Meera’s arm. “It’s understandable to feel that way. The good news is that most blocked tear ducts are harmless and resolve on their own. But there are a few risks to be aware of.”
I explained the potential complications:
- Conjunctivitis (pink eye): When bacteria get trapped, it can lead to an infection with redness, swelling, and yellow-green discharge.
- Dacryocystitis: If the tear duct becomes infected, it can cause swelling near the nose, which may need antibiotics.
- Persistent Blockage: In rare cases, if the duct remains blocked beyond 12 months, a minor procedure may be needed.
Home Treatment Options
I leaned back and smiled reassuringly. “Most of the time, simple home care can help clear the blockage.”
Gentle Massage Technique
I demonstrated the tear duct massage technique on Aarav, using my clean pinky finger.
- Locate the tear duct: It’s at the inner corner of the eye.
- Massage gently downward: With clean hands, use a fingertip to apply gentle pressure from the inner corner of the eye, moving down along the side of the nose.
- Repeat 2-3 times a day: Do this regularly, especially after cleaning away any discharge.
“This helps encourage the tear duct to open and drain properly,” I explained. “It might take a few weeks, but it often works.”
Warm Compresses
I added, “You can also use a warm, damp cloth to gently wipe away any discharge. This can ease discomfort and reduce crusting.”
Meera nodded, her face a bit more relaxed. “I can do that. Is there anything else I should know?”
When to Seek Medical Help
“Yes,” I said gently. “You should bring Aarav back if you notice any of these signs:”
- Redness or swelling around the eye.
- Thick yellow or green discharge that doesn’t improve.
- Fever or signs of discomfort.
- If the blockage doesn’t clear by 12 months.
Medical Treatments
I reassured her that most cases don’t need medical intervention. But if they do, options include:
- Probing Procedure:
A small probe is inserted to open the duct, usually done under light anesthesia. - Balloon Catheter Dilation:
A tiny balloon is used to widen the duct. - Surgery (Dacryocystorhinostomy):
Rarely needed, this procedure creates a new tear drainage pathway.
A Gentle Goodbye
As I wrapped up, I smiled at Meera. “You’re doing a wonderful job, Meera. Aarav is lucky to have such a caring mom.”
She smiled back, a hint of relief softening her eyes. “Thank you, Priya. It helps so much to know what’s going on.”
I waved as she walked out, Aarav’s gurgles echoing softly in the hallway. Moments like these — offering reassurance, turning worry into hope — reminded me why I loved being both a doctor and a part of this community.


