What if the burning sensation you’ve brushed off as “no big deal” could spiral into something far worse? Many people underestimate how quickly bacterial infections in their system can escalate—but early action is critical to avoiding complications.
These infections occur when bacteria invade areas like the bladder, urethra, or kidneys. Left untreated, they can spread and damage vital organs. You might notice pain during urination, frequent urges to go, or cloudy urine. Ignoring these signs often leads to worsening discomfort.
Thankfully, solutions exist. Antibiotics prescribed by a healthcare provider can clear most cases quickly. For milder issues, hydration and cranberry supplements may offer relief. However, self-diagnosing risks delays in proper care.
This guide breaks down how to spot trouble early, effective treatments, and lifestyle changes to reduce recurrence. You’ll also learn why certain groups—like women or those with diabetes—face higher risks. Knowledge empowers you to protect your health before minor irritation becomes a major problem.
Overview of Urinary Tract Infections
Imagine a silent invader creeping into your body’s most critical pathways—undetected until it’s too late. Bacterial disruptions in your filtration network often start small but can rapidly escalate. Recognizing how these issues develop begins with understanding the structures involved and their vulnerabilities.
What Is a UTI and How It Affects Your Body
A urinary tract infection occurs when harmful microbes overpower your natural defenses. E. coli, commonly found in the intestines, is the primary culprit. These bacteria travel upward, attaching to walls of the bladder or urethra. Left unchecked, they multiply and trigger inflammation.
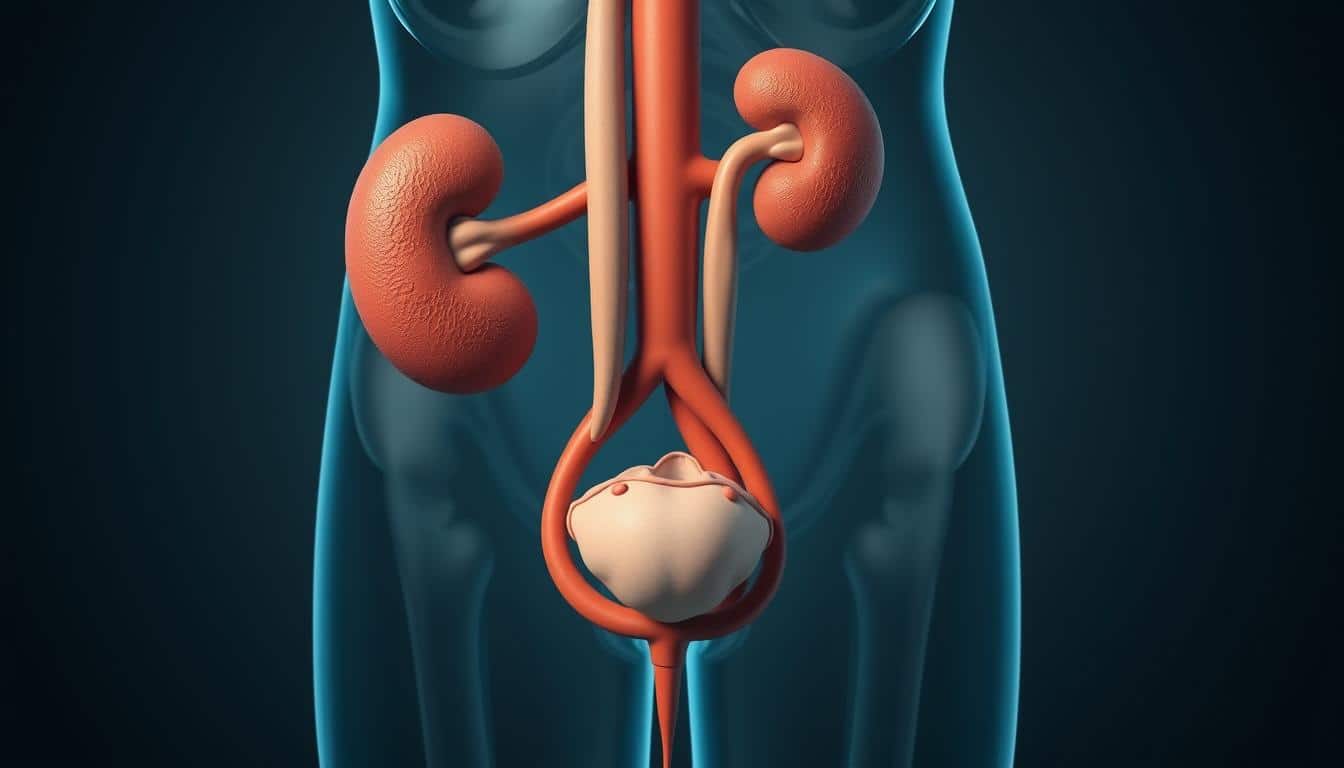
Key Components of the Urinary System
Your body’s waste removal network includes four vital parts. The kidneys filter blood, creating urine. Tubes called ureters carry it to the bladder, which stores fluid until release. Finally, the urethra expels it from your body. Each component must function smoothly to prevent microbial buildup.
Early signs like pelvic pressure or unusual urine color signal trouble. Addressing these quickly helps stop spread to kidneys. Knowledge of this process empowers you to act before minor irritation becomes systemic.
What Triggers Discomfort and How to Find Relief Quickly
Every day, countless individuals face bacterial invasions in their systems—often due to everyday habits. Common triggers include improper hygiene, intimate activity, or even dehydration. When microbes like E. coli migrate from the gut, they cling to urinary pathways, sparking irritation.
Early warning signs demand attention. A persistent urge to urinate, even with little output, often signals trouble. Burning sensations or pelvic pressure may follow, escalating if ignored. Cloudy or strong-smelling urine can also indicate microbial overgrowth.
Pain varies from mild discomfort to intense cramping. Some describe it as a sharp sting during urination, while others feel dull aches in the lower abdomen. Ignoring these cues risks complications like kidney involvement.
To feel better faster, consult a healthcare provider for antibiotics. Over-the-counter analgesics ease pain temporarily. At home, drink water to flush bacteria and try heating pads for cramp relief. Cranberry supplements may hinder bacterial adhesion but aren’t a cure-all.
Acting swiftly on symptoms shortens recovery time. Delaying care allows infections to worsen, making treatment harder. Prioritize your well-being—address discomfort early to restore comfort and prevent recurrence.
Recognizing UTI Symptoms and Warning Signs
When your system sounds the alarm, every minute counts. Subtle changes in bathroom habits or discomfort could signal bacterial overgrowth needing swift attention. Learning to decode these messages helps you act before minor issues escalate.
Red Flags Demanding Immediate Action
A burning sensation during urination often appears first. You might also feel persistent pressure in your pelvis or notice urine that looks cloudy or contains blood. These signs typically emerge early, serving as your body’s plea for help.
When Discomfort Becomes Dangerous
If fever or chills develop alongside lower back pain, the issue may have reached your kidneys. Older adults or children might show confusion, fatigue, or loss of appetite instead of classic symptoms. Never dismiss these variations—they’re equally urgent.
Delaying care for severe signs risks permanent damage. Seek immediate medical evaluation if symptoms intensify or spread. Early intervention stops infections from becoming life-threatening crises.
Risk Factors and Prevention Strategies
Did you know your daily choices could determine whether harmful bacteria gain a foothold? Certain habits and biological factors make some individuals more vulnerable than others. By understanding these triggers, you can build defenses against recurring issues.
Lifestyle Habits to Minimize Your Risk
Women face higher susceptibility due to shorter urethras and proximity to the rectum. Simple adjustments like wiping front-to-back after using the bathroom block bacterial transfer. Opt for cotton underwear and avoid tight clothing—these choices reduce moisture where microbes thrive.
Stay hydrated to flush your system regularly. Holding urine for hours allows germs to multiply. Aim to drink six to eight glasses of water daily and urinate every 2-3 hours.
Practical Prevention Tips and Daily Routines
After sex, empty your bladder immediately to expel potential invaders. Consider avoiding spermicides or diaphragms if you experience frequent issues—these products can disrupt natural defenses.
For people with diabetes or weakened immunity, monitor blood sugar levels closely. High glucose creates favorable conditions for bacterial growth. Incorporate probiotics like yogurt to support healthy gut and urinary flora.
Small, consistent actions form your best shield. Pair smart hygiene with mindful routines to lower your risk significantly over time.
Diagnosis and Testing Procedures
Accurate identification of bacterial issues starts with precise testing methods. Healthcare providers rely on specific tools to confirm suspicions and tailor treatments effectively.
Understanding Urine Tests and Lab Diagnostics
A simple urine sample often holds the answers. Dipstick tests provide instant results by detecting nitrites or white blood cells. For deeper analysis, labs use urinalysis to examine clarity, pH levels, and cellular content.
Culture tests identify the exact bacteria strain causing trouble. This step ensures prescribed antibiotics match the infection type. Advanced scans might be ordered if results suggest issues reaching the kidneys or urethra.
When to Consult Your Healthcare Provider
Persistent discomfort despite home care? Seek professional evaluation immediately. Symptoms like fever or flank pain indicate possible kidney involvement. Recurrent episodes also warrant further investigation.
Timely testing prevents guesswork. Proper diagnosis guides targeted antibiotic use, reducing recovery time and complications. Don’t wait—early action protects your long-term health.
Treatment Options: Antibiotics and Home Remedies
Your body’s alarm bells ring—now what? Addressing microbial invaders requires a two-pronged approach: medical precision and supportive self-care. Combining prescribed treatments with practical home strategies can accelerate healing and reduce discomfort.
Professional Medical Treatments and Antibiotics
Doctors often prescribe antibiotics like trimethoprim or nitrofurantoin to eliminate harmful microbes. These medications target specific bacteria causing inflammation in your bladder or urethra. Completing the full course—even if symptoms fade—prevents lingering germs from rebounding.
For severe cases, especially when kidney involvement is suspected, stronger intravenous antibiotics may be necessary. Always report side effects like nausea or rashes to your provider. They can adjust your regimen to ensure safety and effectiveness.
Effective At-Home Relief Measures
While waiting for antibiotics to work, drink extra water to flush out germs. Aim for eight glasses daily. Over-the-counter pain relievers like phenazopyridine ease burning sensations temporarily—but never use them as a long-term fix.
Some find cranberry supplements helpful, though evidence remains mixed. Heating pads on your lower abdomen may soothe cramping. Remember: these steps support recovery but don’t replace professional care.
Never stop antibiotics early, even if you feel better. Partial treatment allows resilient bacteria to survive, increasing relapse risks. Partner with your healthcare team for lasting results.
Special Considerations for Children, Men, and Older Adults
Your age and biology influence how your body sounds the alarm—and when to listen. While bacterial issues affect all groups, their warning signs and risks vary dramatically. Tailored approaches ensure timely care for those most vulnerable.
Unique Patterns Across Lifespans
Children often show vague symptoms like irritability or fever instead of classic discomfort. Toddlers might avoid using the bathroom or wet the bed unexpectedly. These subtle cues require swift testing to prevent kidney infection progression.
For men, lower incidence doesn’t mean lower risk. When issues arise, they’re more likely linked to prostate enlargement or urinary blockages. Pain during urination or cloudy urine in males often signals complex cystitis needing prompt evaluation.
Older adults face stealthier threats. Confusion, fatigue, or loss of appetite might overshadow typical signs. Weakened immunity raises kidney infection risks, especially in those with diabetes. Postmenopausal women experience increased vulnerability due to estrogen decline.
Prevention strategies adapt to these differences. Cranberry supplements may help women maintain urinary health by blocking bacterial adhesion. Men benefit from prostate checks and hydration, while seniors should prioritize routine screenings.
Seek care immediately if fever accompanies back pain or symptoms persist beyond 48 hours. Early intervention prevents minor cystitis from becoming systemic crises. Your age group dictates your action plan—know yours.
Understanding Chronic and Recurrent UTIs
Recurring battles with infection aren’t just bad luck—they’re clues to hidden microbial strategies. While most cases resolve quickly, some bacteria develop survival tactics that defy standard treatments. Recognizing these patterns helps you break cycles of discomfort before they disrupt your life.
Acute Versus Chronic Infections Explained
Acute infections strike suddenly and typically clear within days of antibiotic use. Chronic cases, however, linger or return repeatedly within months. Research shows certain bacteria form protective biofilms—sticky layers that shield them from medications—within the urinary tract. These hidden colonies resist elimination, causing flare-ups.
A prolonged course of antibiotics (weeks instead of days) may be needed to dismantle persistent microbes. Low-dose maintenance therapy sometimes follows to prevent regrowth. Factors like anatomical abnormalities, weakened immunity, or incomplete prior treatments may also fuel recurrence.
Consult a specialist if infections persist despite initial care. They’ll investigate underlying causes through advanced imaging or urine cultures. Personalized plans—like combining antibiotics with bladder training—often yield better outcomes than generic approaches.
Medications and the Issue of Antibiotic Resistance
Antibiotics save lives, but their power diminishes when misused. Over time, bacteria evolve defenses against these drugs, creating stubborn infections that resist treatment. Understanding how to use medications wisely protects their effectiveness for everyone.
Commonly Prescribed Antibiotics and Their Uses
Amoxicillin and nitrofurantoin are front-line treatments for uncomplicated cases. For stubborn infections, ciprofloxacin may be prescribed. Each medication targets specific bacteria, which is why urine cultures guide choices.
Taking the full course—even after symptoms fade—is critical. Stopping early leaves surviving germs time to adapt. This mistake fuels resistance, making future treatments less reliable.
How to Prevent and Manage Antibiotic Resistance
Always finish prescriptions as directed. If you get UTIs repeatedly, ask about low-dose preventive options. Avoid using leftover antibiotics or sharing them—these habits accelerate resistance.
Stay hydrated with water, not sugary juice, to support medication effectiveness. Cranberry juice lacks strong evidence but may help some people when paired with proper care. Report lingering symptoms to your provider immediately—delays let resistant strains thrive.
Your actions matter. By using antibiotics responsibly, you protect their power for yourself and others. Together, we can outsmart bacterial evolution.
Conclusion
Taking control of your health starts with recognizing subtle changes. Early detection of issues like burning sensations or frequent urges can stop minor irritation from escalating. Acting quickly ensures treatments work effectively and reduces recovery time.
Adopting smart habits helps prevent recurring problems. Stay hydrated, practice proper hygiene, and consider cranberry juice as part of your routine—studies suggest it may block bacterial adhesion. These steps, paired with prompt medical care, form your strongest defense.
Adults, especially those with higher risk factors, should prioritize regular check-ups. Track patterns in discomfort and communicate them to your provider. Knowledge combined with proactive choices empowers you to safeguard your well-being long-term.
Your next move matters. Schedule consultations at the first sign of trouble, and maintain preventive strategies daily. Small actions today create lasting protection against tract infections tomorrow.