Could a lingering cough be more than just a cold? This question haunts many who brush off fatigue or a sore throat as seasonal annoyances. What feels like a minor bug might actually signal a stealthy respiratory condition requiring attention.
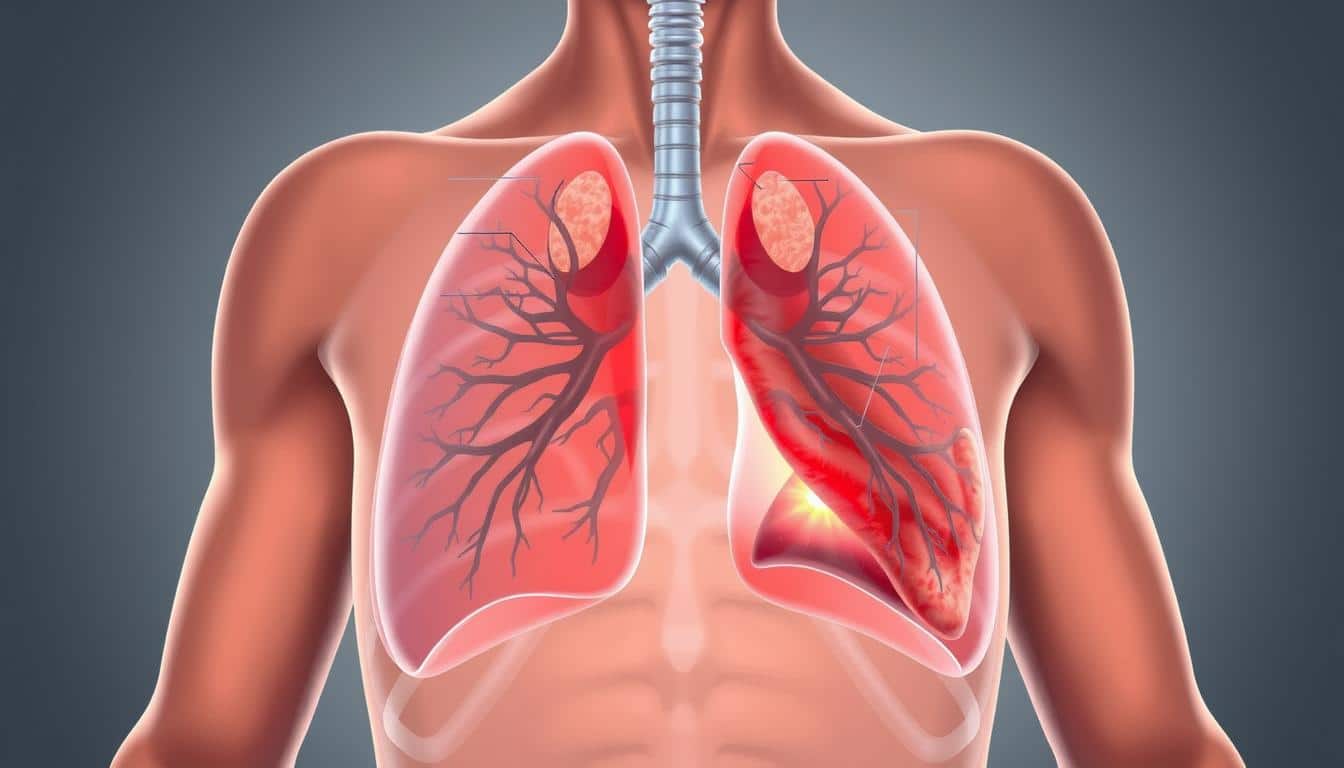
Often called “atypical pneumonia,” this infection targets lung tissue with subtlety. Unlike traditional pneumonia, it rarely causes severe fever or hospitalization—yet ignoring it risks complications like bronchitis or chronic respiratory strain. The CDC notes that both bacteria and viruses trigger cases, with antibiotics effective for bacterial forms.
Many mistake early signs for common illnesses, delaying care. A dry cough that persists for weeks, low-grade fatigue, or mild chest discomfort often fly under the radar. Left unchecked, however, these indicators can escalate. Early diagnosis speeds recovery and reduces contagion risks, especially in crowded spaces or schools.
This article unpacks how to spot red flags, navigate treatment options, and safeguard your health. You’ll learn why quick action matters, how to differentiate this condition from routine colds, and what steps experts recommend for prevention. Let’s explore how to stay ahead of an infection that thrives on being overlooked.
Understanding Walking Pneumonia: A Mild Infection with Serious Risks
A sore throat that lingers could be hiding a stealthy invader. Often termed “atypical pneumonia,” this condition creeps into lung tissue without dramatic warning signs. Unlike its traditional counterpart, it’s frequently traced to Mycoplasma pneumoniae bacteria and thrives where crowds gather—schools, offices, or public transit.
What Is This Stealthy Lung Condition?
This infection primarily strikes those aged 5 to 35. While labeled “walking pneumonia,” don’t let the nickname fool you. Chest scans reveal scattered inflammation patterns rather than dense lung consolidation. You might feel well enough to continue daily activities, but your body fights a hidden battle.
Spotting the Differences
Standard pneumonia often brings high fever and mucus-heavy coughs. With atypical cases, symptoms like dry hacking or low-grade fatigue dominate. Viruses sometimes trigger similar issues, but bacterial origins require specific antibiotics. Delayed care allows the problem to deepen, making early detection critical.
Schools and dorms become hotspots due to close contact. Shared surfaces and airborne droplets spread the bacteria through coughs or sneezes. While most recover fully, untreated cases may strain the heart or worsen existing respiratory conditions. Knowledge remains your best defense against this quiet threat.
Symptoms and Early Warning Signs
That tickle in your throat might seem harmless, but when paired with fatigue, it could signal more than seasonal sniffles. Early indicators often mirror routine illnesses, making them easy to dismiss. Research shows 40% of cases initially get mistaken for colds, delaying proper care.
When a Cold Isn’t Just a Cold
A dry hack that lingers beyond three weeks separates this condition from typical viruses. You might notice a slight temperature—99°F to 101°F—that comes and goes. Sore throats and headaches often join the mix, creating a misleadingly mild profile.
Children frequently experience these issues during school months. Their energy levels may dip, yet they continue attending classes. This “keep going” tendency allows the infection to spread silently among peers.
Hidden Clues in Your Body
Chest tightness when breathing deeply warrants attention—it suggests lung irritation. Daytime tiredness that coffee won’t fix could mean your system is fighting harder than it admits. Night sweats or appetite loss sometimes appear weeks after initial exposure.
Clinicians urge monitoring patterns: if complaints intensify after five days, seek evaluation. Antibiotics work best when started early, preventing bronchitis or asthma flare-ups. Don’t let a “manageable” cough trick you—silent threats demand proactive responses.
Risk Factors and Who Is Most Vulnerable
Your daily environment might be quietly heightening health risks. Crowded spaces accelerate germ spread, but personal health history often determines who develops complications. Those with chronic respiratory conditions face amplified danger—their lungs already work overtime before infection strikes.
Underlying Conditions and Age Groups
Asthma and COPD patients are 3x more likely to experience severe outcomes, per Johns Hopkins research. Immune-compromised individuals—including cancer patients or organ transplant recipients—struggle to contain initial infections. Even past lung damage from smoking increases vulnerability.
Age plays a critical role. Children under 12 lack fully developed immune defenses, while adults over 65 face natural decline in respiratory function. Surprisingly, 20-40 year-olds account for 45% of cases due to workplace exposure and social activity levels.
Prevention becomes non-negotiable for these groups. Annual flu shots reduce secondary infections, and mask use in airports or classrooms blocks transmission routes. Early testing matters most when risk factors align—don’t wait for chest tightness to become unbearable.
Diagnosis and Testing Options
Persistent discomfort when breathing deeply deserves more than a dismissive shrug. Healthcare providers use a combination of physical checks and advanced tools to uncover hidden respiratory issues. Early detection ensures targeted treatment and prevents complications.
Physical Exams and Imaging
Your doctor will first listen to your chest using a stethoscope. Crackling or wheezing sounds often hint at inflammation in the lungs. These clues guide further investigation.
Chest X-rays reveal scattered patches of infection instead of solid areas. This pattern helps distinguish atypical cases from standard pneumonia. Imaging also rules out other conditions with similar signs.
Laboratory Tests and What to Expect
Blood tests identify markers of bacterial or viral activity. A throat swab might be collected to detect mycoplasma or other pathogens. These results pinpoint the exact cause of your infection.
Some clinics use rapid tests for quicker answers. If your cough persists despite rest, lab work becomes essential. Timely analysis speeds up prescription decisions—like choosing the right antibiotics.
Testing takes minutes, but results may require 24-48 hours. Share all signs openly, even mild fever or fatigue. Your honesty helps professionals connect subtle dots.
Treatment and Management: Your Options for Recovery
Your path to healing begins with understanding available treatments. While walking pneumonia often resolves on its own, targeted strategies speed recovery and prevent setbacks. Both medical interventions and self-care play vital roles in restoring lung health.
Antibiotics and When to Use Them
Doctors prescribe antibiotics like azithromycin when tests confirm bacterial involvement. These medications stop Mycoplasma pneumoniae from multiplying, easing coughs within days. Viral cases won’t respond—rest becomes the primary therapy.
Complete the full course even if you feel better sooner. Stopping early risks antibiotic resistance. Report side effects like nausea promptly—your provider can adjust dosages or switch medications.
Home Care and Over-the-Counter Remedies
Hydration thins mucus, while ibuprofen reduces low-grade fever. Use cough suppressants sparingly—your body needs to clear irritants. A cool-mist humidifier soothes raw airways overnight.
Prioritize sleep and avoid overexertion. Light activity is fine, but pushing too hard delays recovery. Track symptoms daily—if breathing worsens after five days, contact your clinic immediately.
Most patients improve within 2–3 weeks with proper care. Combine prescribed antibiotics with smart home habits to outpace this stealthy infection.
Preventative Measures and Practical Health Tips
Your daily routine holds the key to staying one step ahead of respiratory threats. Simple adjustments can build defenses against infections while helping you recognize when professional guidance becomes essential.
Daily Habits to Strengthen Your Immune System
Start with thorough handwashing—scrub for 20 seconds after touching shared surfaces. Pair this with a diet rich in citrus fruits and leafy greens to fuel your body’s natural armor. Regular exercise, even light walks, improves lung capacity and circulation.
Prioritize 7–9 hours of sleep nightly. Rest allows your system to repair and recharge. Hydration matters too—water flushes toxins and keeps mucous membranes resilient.
Guidelines on When to Seek Medical Advice
Contact your doctor if a cough lasts over 10 days or breathing feels strained. Watch for sudden fever spikes or chest pain that disrupts daily tasks. These signs often demand swift care to prevent complications.
Annual flu shots reduce overlapping infections that weaken defenses. Avoid crowded spaces during peak illness seasons—virtual meetings or outdoor gatherings lower exposure risks. When prevention fails, early treatment stops minor issues from becoming major battles.
Remember: Proactive care keeps you safer than reactive solutions. Track changes in your health like an investigator—small clues often reveal big truths.
Walking Pneumonia: Mild Symptoms, Serious Risks – What You Need to Know
Behind every persistent cough lies a microscopic culprit. Mycoplasma pneumoniae, a unique bacterium, drives most cases of this respiratory condition. Unlike typical germs, it lacks a cell wall—making it resistant to common antibiotics like penicillin.
Understanding the Bacterial Causes and Infections
This pathogen primarily targets your throat and airways. It attaches to lung tissue, slowly damaging the lining over weeks. The CDC reports a 15% rise in M. pneumoniae cases last year, particularly in school-aged children and young adults.
Transmission happens through close contact. Shared airspace during conversations or a sneeze in crowded rooms spreads the bacteria. Once inhaled, it incubates for 1–4 weeks before triggering that nagging cough.
Viral respiratory issues often resolve faster. Bacterial infections linger, sometimes leading to ear inflammation or asthma exacerbations. While 70% of cases stay mild, untreated infections may progress to pleural effusions—fluid buildup around lungs.
Outbreaks peak every 3–7 years, especially in late summer and fall. Schools and military barracks see clusters due to shared living spaces. Recognizing these patterns helps health officials contain outbreaks before they escalate.
Antibiotics like doxycycline or azithromycin effectively treat bacterial forms. Early intervention prevents complications, but misdiagnosis remains common. If your cold-like symptoms drag on, ask about specific testing for this stealthy invader.
Living with Walking Pneumonia: Coping and Recovery Strategies
Recovering from this respiratory illness requires balancing rest with smart daily adjustments. While antibiotics tackle bacterial mycoplasma cases, your habits determine how quickly you regain strength. Let’s explore practical ways to ease discomfort and prevent setbacks.
Steps to Help You Feel Better Faster
Start by prioritizing sleep—your body heals best during deep rest. Set reminders to drink water hourly, as hydration thins mucus and protects lung tissue. Warm broths and herbal teas soothe irritated airways while providing essential nutrients.
Track symptom changes in a journal. If your cough worsens after 10 days or fatigue disrupts basic tasks, contact your doctor immediately. Most cases improve within 2–3 weeks, but delayed care risks hospitalization.
Follow prescribed medications precisely, even if energy returns early. Over-the-counter pain relievers reduce low-grade fevers, but avoid suppressants that block productive coughing. Use a humidifier nightly to maintain moist air—this prevents throat dryness and promotes easier breathing.
Gradually reintroduce activities. Short walks boost circulation without overexertion. Don’t push through fatigue—your immune system needs reserved energy. Shield yourself from stress by delegating tasks and setting clear recovery boundaries.
These strategies help most people overcome walking pneumonia without complications. Consistency matters more than speed—listen to your body’s signals and adjust your pace accordingly.
Conclusion
Ignoring persistent discomfort could mask a hidden respiratory challenge. Walking pneumonia, often mistaken for common colds, quietly affects lung function with subtle symptoms like lingering coughs or fatigue. Early detection through chest exams and targeted testing prevents complications, especially in crowded environments where infections spread rapidly.
Effective care combines prescribed antibiotics with rest and hydration. While most cases resolve without hospitalization, delayed treatment risks prolonged recovery. Adults and children benefit from preventive habits—frequent handwashing and monitoring throat irritation. Over-the-counter remedies may ease discomfort but consult a doctor first.
Stay alert to persistent symptoms. Adequate bed rest supports recovery if diagnosed. Consult a provider if issues linger beyond 10 days. Walking pneumonia demands attention, not alarm. Proactive measures reduce your chance of getting walking pneumonia.
Remember: proper care stops this condition from disrupting daily life. Prioritize well-being—knowledge and action defend against getting walking pneumonia’s stealthy advance.