What if that nagging discomfort in your gut isn’t just a passing issue? While most people brush off occasional bellyaches, understanding their origin could be the key to safeguarding your health. Discomfort between your ribs and pelvis can range from dull cramps to sharp stabs—and how you describe it often depends on your unique experience.
This type of unease is incredibly common. Nearly everyone faces it at some point, whether from indigestion, stress, or minor infections. But here’s the twist: not all sensations are created equal. Some fade quickly, while others signal deeper problems needing expert care.
Why does this matter? Ignoring persistent or severe symptoms might delay critical treatment. This guide breaks down what you need to know—from everyday triggers to red flags that demand a professional’s insight. You’ll learn how to distinguish routine discomfort from urgent health concerns and when it’s time to take action.
Ready to decode your body’s signals? Let’s explore the possibilities—and empower you to make informed decisions about your well-being.
Understanding Abdominal Pain
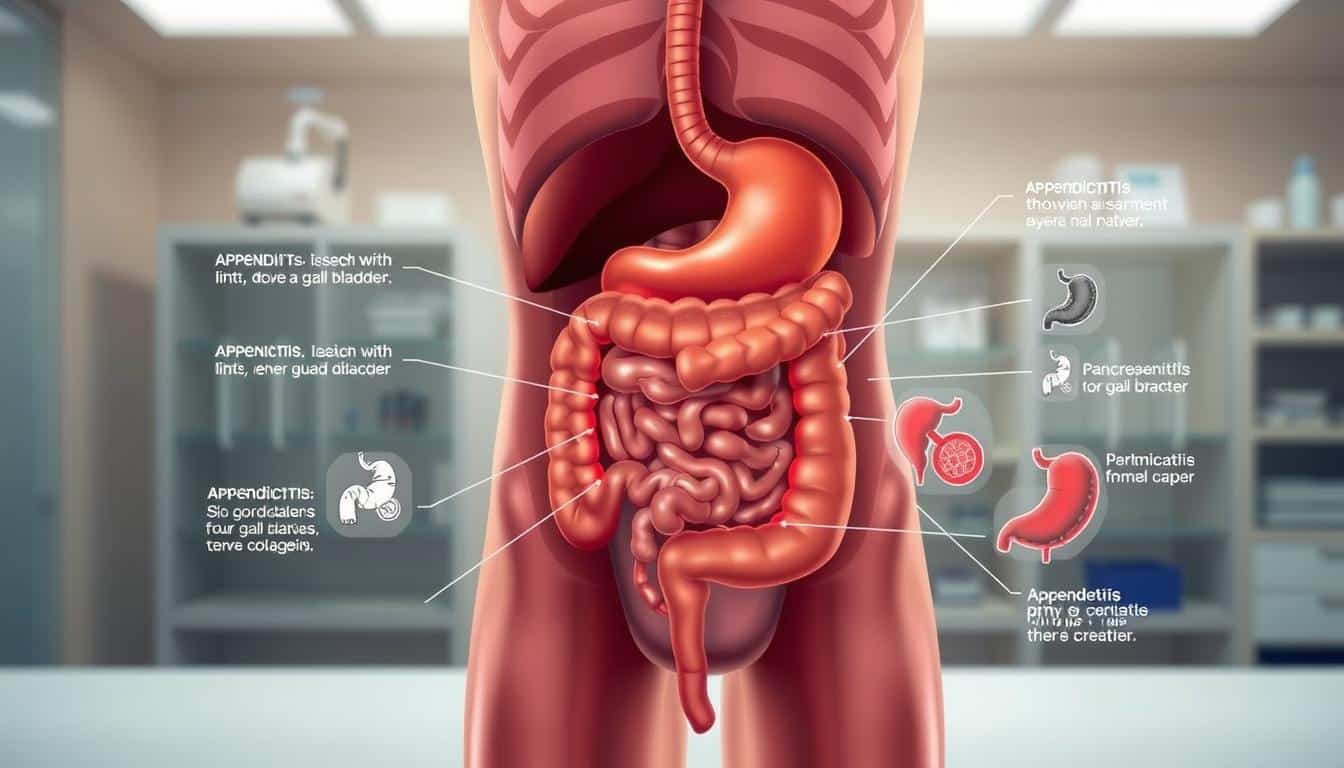
Many people use “stomach pain” to describe any discomfort in their belly. However, this area houses more than just your stomach. The abdomen stretches from below your chest to your pelvis, containing organs like the liver, intestines, and pancreas. Pinpointing where your sensation originates helps identify potential issues.
What You Need to Know About Pain in Your Belly
True stomach pain typically centers in the upper left area, beneath the ribs. It often links to indigestion or acid reflux. But discomfort elsewhere might signal problems in other organs. For example, cramping near your navel could stem from intestinal issues, while right-side tenderness might involve the appendix.
Differences Between Stomach Pain and Abdominal Discomfort
While the terms are often used interchangeably, they’re not the same. Causes abdominal pain vary widely—gallstones, kidney infections, or even muscle strains. Your brain may struggle to distinguish these sources, leading to similar sensations from different triggers. Sharp twinges near your ribs could relate to the gallbladder, whereas lower pelvic pressure might indicate bladder concerns.
Recognizing these patterns helps you decide when to monitor symptoms or seek care. If discomfort persists or worsens, professional evaluation becomes critical.
Symptoms and Variations of Abdominal Pain
Your body communicates through sensations that range from barely noticeable to impossible to ignore. These signals often differ in intensity, duration, and quality—each offering clues about their origin. Understanding these variations helps you gauge whether discomfort is manageable at home or requires urgent evaluation.
Mild, Moderate, and Severe Pain
Mild twinges often resolve with rest or hydration, like bloating from dietary choices. Moderate discomfort—such as persistent cramping—might suggest infections or digestive irregularities. Severe episodes, especially paired with fever or vomiting, could indicate emergencies like appendicitis or intestinal blockages.
Intensity alone doesn’t always dictate urgency. For example, kidney stones might start as a dull ache before escalating rapidly. Track how symptoms evolve over hours. Sudden changes in pain severity often demand faster action.
Dull, Sharp, and Crampy Sensations
A dull, gnawing sensation frequently points to inflammation, such as gastritis. Sharp, stabbing pains may signal ulcers or gallstones. Crampy waves—common with constipation or menstrual cycles—often ease with movement or warmth.
Notice accompanying signs: nausea with sharp pains might indicate pancreatitis, while diarrhea alongside cramps could mean foodborne illness. These patterns help doctors prioritize tests like blood work or imaging to pinpoint causes efficiently.
Anatomy of Your Abdomen and Pain Sources
Your torso holds a complex network of structures working together to process nutrients and eliminate waste. The area spans from your diaphragm to the pelvic bones, divided into four quadrants for medical evaluation. Each zone correlates with specific organs—a map your doctor uses to trace symptoms back to their source.
Key Organs Involved in Digestive Health
The stomach breaks down food using acids, while the small intestine absorbs nutrients. Your large intestine—or bowel—processes waste before elimination. When inflamed or blocked, these organs trigger distinct discomfort patterns. For example, upper midline burning often points to gastric issues, whereas lower cramping may signal bowel irregularities.
Other Structures Contributing to Pain
Muscles, nerves, and connective tissues in the abdominal wall can also generate sensations. A strained muscle might mimic internal organ distress but eases with rest. Even skin conditions like shingles cause localized tenderness. This explains why some “deep” aches actually stem from surface layers.
Recognizing these relationships helps you describe symptoms accurately. Sharp twinges near the ribs could involve the liver or gallbladder, while pelvic pressure might relate to bladder function. Location matters—it guides diagnostic priorities and treatment plans.
Abdominal Pain: Common Causes and When to See a Doctor
Digestive disturbances and organ-related issues account for most belly-related complaints. From temporary upsets to chronic conditions, identifying the source guides your next steps. Let’s explore frequent triggers and when they demand expert attention.
Gastrointestinal and Kidney-Related Conditions
Stomach viruses and foodborne infections often trigger cramping and diarrhea. These usually resolve within days. However, sharp right-lower quadrant pain could signal appendicitis—requiring immediate care to prevent rupture. Gallbladder inflammation causes intense upper-right discomfort, especially after fatty meals.
Kidney stones create waves of flank pain radiating to the groin. Urinary urgency or blood in urine often accompanies these episodes. Chronic kidney issues may cause dull aches paired with fatigue or swelling.
Infections, Inflammatory Diseases, and More
Persistent diarrhea or bloody stools might indicate inflammatory bowel disease like Crohn’s. These conditions often flare unpredictably, needing long-term management. Untreated bacterial infections can spread, causing sepsis—a life-threatening response.
Seek help if pain lasts over 48 hours or includes fever, vomiting, or inability to eat. Sudden worsening or inability to find relief through rest also warrants evaluation. Early intervention prevents complications from escalating causes like blocked intestines or infected organs.
Differentiating Acute, Chronic, and Progressive Pain
The clock matters more than you think when discomfort strikes. How long symptoms last—and whether they intensify—can reveal critical details about their origin. Recognizing these patterns helps you decide whether to wait it out or contact a healthcare provider.
Identifying Acute Versus Chronic Pain
Acute sensations flare suddenly and often resolve within hours or days. Think food poisoning or muscle strains. These types abdominal issues usually respond to rest or hydration. Chronic discomfort, however, lingers for months. Conditions like irritable bowel syndrome or endometriosis often follow this pattern.
Time plays a key role here. If your symptoms persist beyond two weeks without improvement, it’s worth investigating. The cause might involve inflammation or nerve sensitivity requiring targeted treatment.
Recognizing Progressive Patterns
Progressive pain grows steadily worse, signaling escalating issues like infections or tumors. For example, a dull ache that sharpens over days could indicate appendicitis. Notice if basic activities like eating or moving worsen your condition.
Tracking how your sensations evolve helps pinpoint the cause abdominal pain. Sudden weight loss paired with escalating cramps? These combinations often demand imaging tests or blood work. Don’t dismiss gradual changes—they’re your body’s way of sounding alarms.
Diagnostic Approaches and Evaluation
Doctors use a toolbox of strategies to uncover why you’re feeling unwell. They start by gathering clues through conversation and hands-on checks before ordering targeted tests. This systematic approach ensures nothing gets overlooked.
Physical Examinations and Patient History
Your provider will press gently on different belly areas, asking where it hurts most. They’ll listen for bowel sounds and check for tenderness that shifts with movement. Sharing details about recent meals, travel, or stress helps them connect dots between symptoms and potential triggers.
Imaging, Endoscopy, and Laboratory Tests
Blood tests reveal infections or inflammation, while urine analysis spots kidney issues or dehydration. If stones are suspected, a CT scan visualizes the urinary tract. Ultrasound checks gallbladder or liver problems without radiation.
For persistent upper belly discomfort, an endoscopy camera examines your stomach lining. Sometimes, chest X-rays rule out lung conditions mimicking digestive pain. These tools work together like puzzle pieces—each test narrowing down possible causes.
Specialized tests kick in when routine results stay unclear. A HIDA scan tracks bile flow, while MRIs detail soft tissues. Your care team prioritizes methods that balance accuracy with minimal invasiveness, ensuring you get answers—not just procedures.
When to Seek Medical Attention
How do you know when discomfort crosses into danger territory? While minor twinges often resolve with rest, certain patterns demand swift action. Recognizing these signals could prevent complications and guide you toward timely solutions.
Critical Warning Signs and Symptoms
Seek care immediately if you experience:
– Pain so intense it disrupts breathing or movement
– Black stools or vomiting blood
– Fever above 101°F with abdominal tenderness
– Sudden swelling or hardness in your belly
These red flags often indicate internal bleeding, severe infection, or organ rupture. Conditions like appendicitis or bowel obstructions worsen rapidly without treatment. If symptoms strike after trauma or alongside chest pressure, head to the ER.
When Home Care Isn’t Enough
Mild cramps from indigestion might ease with hydration and heat. But if symptoms persist beyond 48 hours—or return frequently—see a doctor. Persistent nausea, unexplained weight loss, or pain that spreads to your back also warrant evaluation.
Home remedies fail when underlying disease drives the issue. For example, gallstones require medication or surgery, not just dietary changes. Trust your instincts: if rest doesn’t help or discomfort disrupts daily life, professional care becomes essential.
Treatment Options and Home Remedies
Managing discomfort often starts with understanding your options. From quick fixes to long-term solutions, treatment plans vary based on what’s causing your symptoms. Let’s explore strategies that bring relief while addressing root issues.
Medication and Non-Surgical Approaches
Over-the-counter remedies like antacids or simethicone tackle gas and indigestion effectively. For cramping, heating pads or gentle stretches often ease tension. Staying hydrated with water helps flush irritants from your system—especially during bouts of diarrhea.
Diet plays a key role. Avoiding foods like beans, broccoli, or carbonated drinks reduces bloating. Peppermint tea or ginger supplements may calm spasms naturally. These steps work best when paired with rest and stress management.
When Surgery May Be Necessary
Some conditions demand more aggressive treatment. Appendicitis, severe gallstones, or intestinal blockages often require surgery to prevent complications. Surgeons might remove damaged tissue or repair hernias through minimally invasive techniques.
Doctors typically reserve operations for cases where medications fail or risks escalate. For example, recurring kidney stones might need lithotripsy if dietary changes don’t help. Always follow your provider’s guidance—they’ll tailor plans to your specific needs.
Lifestyle Factors, Prevention, and Self-Care
Your daily choices shape how your body feels—and reacts—to potential triggers. Small, consistent changes often make the biggest difference in supporting your belly’s well-being. Let’s explore practical strategies to maintain comfort and reduce recurring issues.
Dietary Considerations and Food Triggers
What you eat directly impacts digestive health. Spicy foods, dairy, and carbonated drinks rank high as common irritants. Try eliminating one group at a time to identify culprits. High-fiber choices like oats and bananas often soothe sensitive systems.
Portion control matters too. Overeating strains your gut, while regular small meals ease digestion. Keep a food journal—it reveals patterns linking meals to belly discomfort. Hydration is key: aim for eight glasses of water daily to keep things moving smoothly.
Exercise, Hydration, and Daily Habits
Movement isn’t just for fitness—it stimulates digestion. A 20-minute walk after meals can prevent bloating. Yoga poses like child’s pose gently massage internal organs, easing tension.
Stress management also plays a role. Deep breathing exercises lower cortisol levels, reducing inflammation linked to bowel disease. Prioritize sleep—poor rest disrupts gut bacteria balance, increasing sensitivity.
Simple swaps work wonders. Replace sugary snacks with nuts or yogurt. Set phone reminders to drink water. These habits build resilience against flare-ups while boosting overall health.
Proactive care isn’t about perfection—it’s progress. Every positive choice strengthens your body’s defenses against belly troubles. Start with one change today, and let consistency guide your journey.
Conclusion
Your body’s signals hold vital clues about your well-being. Discomfort in your midsection can stem from dozens of sources—ranging from temporary indigestion to urgent conditions needing swift care. Recognizing patterns in intensity, location, and duration helps identify the cause abdominal issues more accurately.
Track how sensations evolve. Mild cramping after meals differs sharply from unrelenting tenderness paired with fever. Diagnostic tools like imaging tests and blood work help doctors pinpoint the underlying cause abdominal distress, whether it’s gallbladder inflammation or intestinal irregularities.
Never dismiss persistent symptoms. While rest and hydration resolve many cases, escalating issues demand professional evaluation. Modern medicine offers tailored treatments—from lifestyle adjustments to minimally invasive procedures—that address root problems rather than just masking discomfort.
Use this knowledge to advocate for your health. If sensations disrupt daily life or match critical warning signs, seek care immediately. Early intervention often prevents complications, empowering you to reclaim comfort and confidence. Your vigilance today could safeguard your tomorrow.